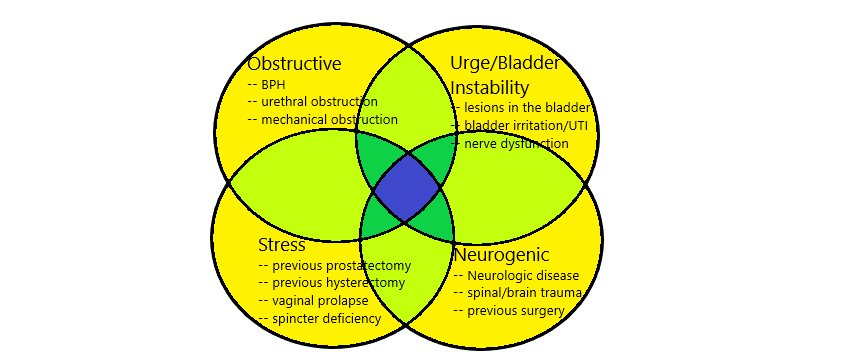
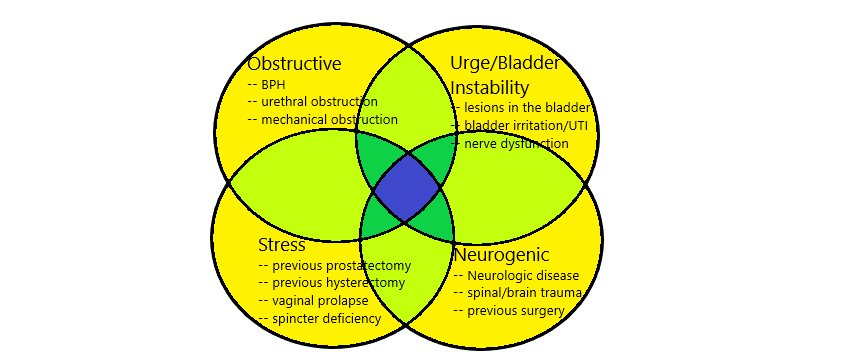
However, when it leads to urinary frequency that becomes bothersome to a person’s life, that is when we start considering treatment. Urge incontinence can be a sign of another more serious issue within the bladder, such as a urinary tract infection, a bladder stone, or even a bladder tumor. Also, it can be debilitating, leading to affected women and men to be imprisoned in their homes because anywhere they go they need to use a restroom, or worry about urine soiling their clothes when they leave the house.
It is important for your urologist to determine the cause of the symptoms, as sometimes urge incontinence can be the first sign of another disease process. Also, it is important for your urologist to determine what other causes may be contributing to the urinary symptoms, as there can be (and often is) more than one contributing reason. You can help your urologist by providing a bladder diary, this can be a very useful tool to determine what kind of incontinence is going on and what can be done about it:
https://www.urologyhealth.org/resources/bladder-diary
For more information on the reason why the body reacts the way it does to cause urge incontinence, please follow the link below
https://www.urologyhealth.org/urology-a-z/o/overactive-bladder-(oab)
Causes of Urinary Symptoms
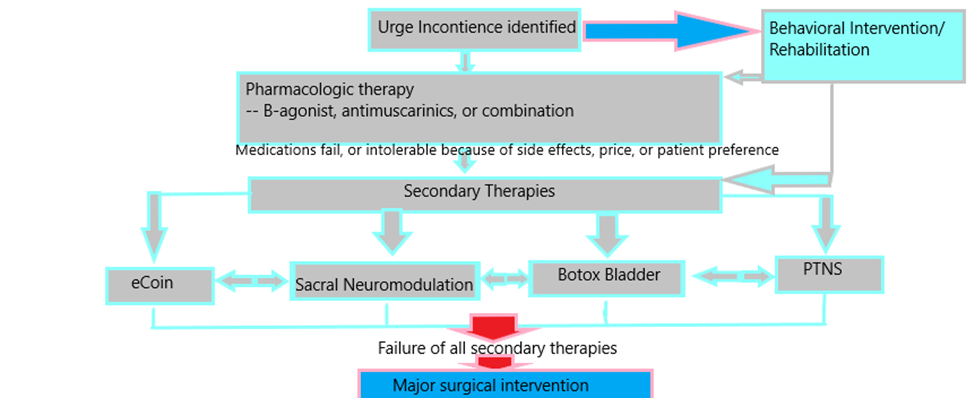
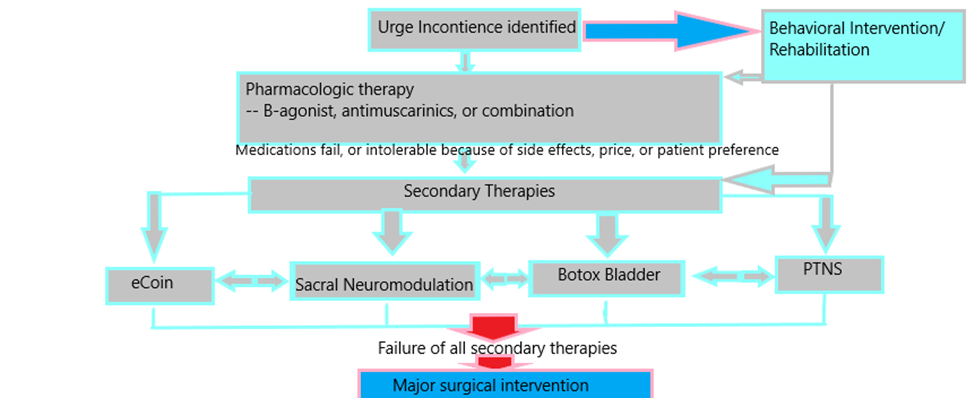
Treatments for urge incontinence include behavioral therapies, medications, in-office procedures, and surgeries performed in an outpatient setting as well as in the hospital.
Behavioral Therapies
There are many exercises and forms of pelvic rehabilitation that can be used to help with urge incontinence symptoms. Often times a urologist will have a therapist, either a pelvic floor physical therapist or a nurse trained in physical therapy, that will be available to help with these symptoms, especially if it is combination with stress incontinence. Pelvic floor therapy can be in the form of exercises, with the help of sensors using biofeedback, or with stimulation methods by direct or electric stimulation of the muscles that may help to control urge symptoms. For more specific recommendations on exercises, and information about incontinence in general, follow the below link:
https://www.urologyhealth.org/healthy-living/care-blog/kegel-exercises-for-incontinence
Pharmacologic Treatments
There are many medications that can be useful to help with urge incontinence. There are two major classes of medications:
Antimuscarinics
These represent the older class of medications to control urge incontinence. They work by inhibiting the contraction of the bladder. Examples are oxybutynin, Detrol, Enablex, Vesicare, trospium, though there are others as well. The main side effects are dry mouth and constipation. These medications also appear on the Beers Criteria Medication list, which are medications that are potentially harmful in the elderly because of worsening dementia. If there is a history of dementia, generally these medications are frowned upon to use.
Beta-adrenergic agonists
These medications are a newer form of medication for urge symptoms. They work by actively promoting relaxation of the bladder rather than inhibiting contraction like antimuscarinics. The two types medications can be used together as a result, which can have more effect than one or the other, but the worry with that is that you can inhibit function of the bladder too much and cause urinary retention, the inability to urinate at all.
Examples of these medications include Myrbetriq and Gemtesa. Because these medications are newer, they tend to be more expensive and insurance generally does not cover them as well. The side effects of these medications are less than antimuscarinics. The most common side effect is an increase in blood pressure, which you may notice as a headache.
Secondary Interventions
For patients that medications don’t work, don’t work well enough, or simply do not want to take medications for cost or fear of side effects, there are other alternatives. There are many interventions that can be performed to alleviate symptoms that can be more effective than medications. Here are the treatment options available.
Bladder Botox
Botox is now so common in various aspects of medicine and cosmetics that it seems most people have at least a passing understanding of the intervention. In the bladder, it can be used to inhibit contractions of and alleviate urge incontinence. It can also be used for neurogenic bladder for a similar purpose.
The procedure is performed by inserting a cystoscope into the bladder, and then injecting small amounts of botox below the surface of the bladder. This is done in an even distribution, and generally the procedure takes about 5-10 minutes to perform. There can be bleeding in the bladder from the procedure, especially if the patient is on blood thinning medication. It becomes necessary sometimes to use a device that electrocauterizes bleeding in the bladder after injections for this purpose.
Like other implementations of botox, the effect wears off generally after 6 months, though there is some variation. As such, for effective treatment, optimal use is at least twice a year. Botox application can be done in the office, though sometimes for comfort it is done in an ambulatory surgery setting. Since the mechanism of action is to inhibit contractions of the bladder, occasionally the bladder can stop contracting altogether, in which case the patient has to wear a catheter or insert a catheter intermittently (a process known as CIC, or clean intermittent catheterization) to allow for urine to flow. Other common risks are bleeding, as noted above, and infection.
Pretibial Nerve Stimulation
Pretibial nerve stimulation, or PTNS, is a procedure where the physician takes advantage of an interesting common nerve pathway to control bladder contractions. The tibial nerve happens to leave the spinal canal in a similar nerve route as the innervation to the bladder. This allows for the tibial nerve, when stimulated, to stimulate and therefore potentially regulate the nerve impulses going to the bladder.
https://www.yourpelvicfloor.org/conditions/percutaneous-tibial-nerve-stimulation-ptns/
This regulation of bladder control by stimulating sacral nerves can be very effective to inhibit abnormal, unintended contractions of the bladder and help normalize urgency and urge incontinence. It forms the basis of PTNS, as well as eCoin neural modulation and sacral neuromodulation.
In PTNS, a site behind the ankle is identified in the office through localization and patient feedback that can be effective in controlling bladder stimulation. The site is marked, and the patient returns weekly for the first 4-6 weeks to get a session of stimulation, then needs to return monthly for stimulation to be effective in controlling symptoms. Risks are minimal, and including bleeding and pain at the site of stimulation, which are rare.
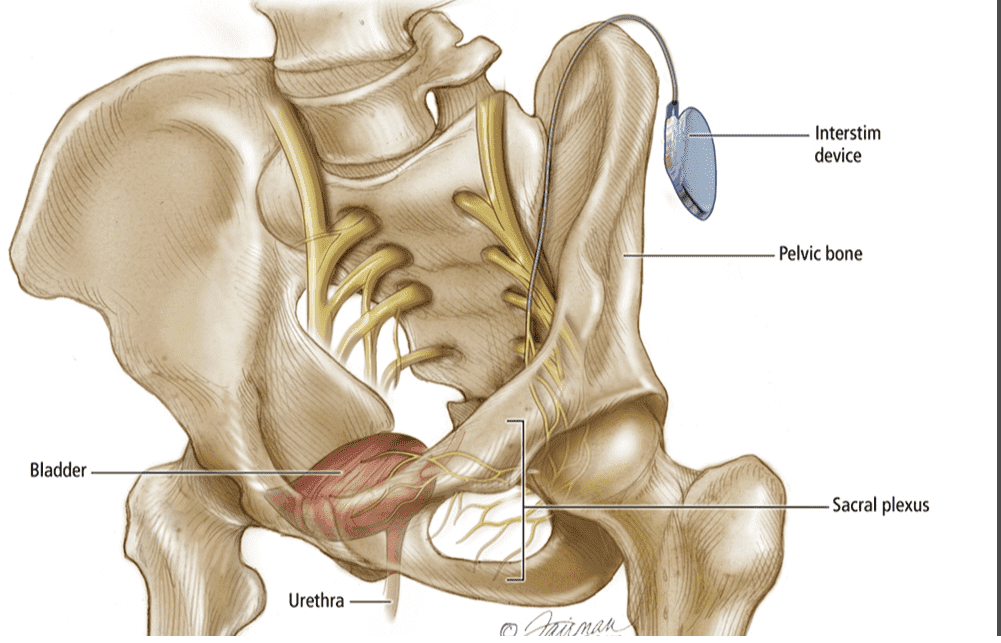
Sacral Neuromodulation
In a similar manner, the sacral nerve can be stimulated directly by sacral neuromodulation. In this procedure, there is first a test phase that is done under local anesthesia to potentially identify the correct location and efficacy of stimulating the sacral nerve. This process is known as a percutaneous nerve evaluation, and the patient is lying flat on his or her belly while the lower back is prepared in a sterile field. Often with the help of live x-ray, the location of the correct sacral nerve is identified with the concurrent aid of a needle and a small pulse of electrical stimulation. Once the patient feedback is what we expect or hope, that needle is used to pass a very small wire on top of the desired nerve. This wire is known as a lead. Most times we do this on both sides to assess which side has a better response. Once established, these wires are attached to a small portable computer that uses these wires to stimulate the nerve and inhibit unwanted contractions. This is carried generally for a week, and if it helps to control urge symptoms to a desirable degree, the patient is considered a candidate for implant.
The implant is done as a separate procedure in the ambulatory surgery setting. The same process is used to place the wire, though this is usually done only on the side that had the best response and/or was the easiest to access. Once the patient has a positive response, he or she is put deeper to sleep and a long-lasting stimulator implant – which consists of a battery and a small computer that can respond to different programs and adjust strengths of stimulation – is placed under the skin. It is something like putting in a pacemaker for the bladder.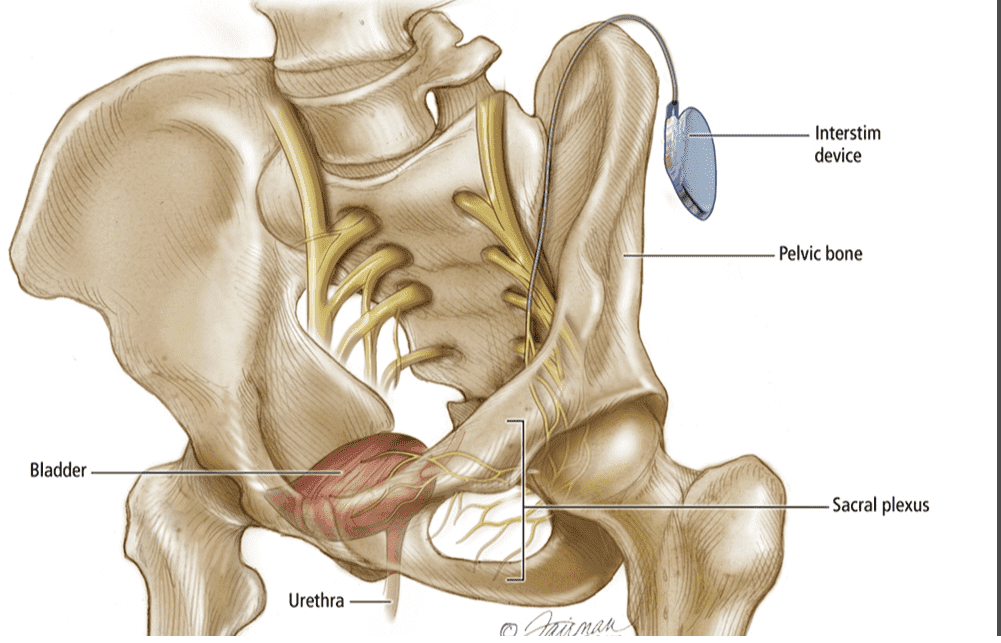
The above is what’s known as a combined stage I and II implant. Alternatively, some patients have a testing period where the results where unclear, or the patient is not able to give a good response of whether there was an adequate response, or the physician is more comfortable with a different approach. In this case, a stage I implant can be performed, where the physician places the lead as if he were putting in the stimulator, but attaches it to a temporary stimulator like the percutaneous nerve evaluation. If it works, the patient is then brought back to the OR for implantation of the battery/stimulator. If it doesn’t, everything is removed. This can allow for a longer testing period, but requires two trips to the operating room.
Risks of the procedure are pelvic pain, loss of efficacy, infection of the implant, misplacement of the lead, and bleeding. This is considered a minimally invasive procedure however, and can be very effective in controlling symptoms. There are two companies that make the stimulators, and two types of implants. One is a rechargeable implant, which can last longer and is smaller but has to be recharged weekly by placing a charging disk on the skin near where the implant is, like wireless charging for a mobile phone. The other option is a semi-permanent battery that generally lasts around 5 years, though recent advances have extended the life of this battery. The stimulator is then replaced in the operating room once stimulation is no longer achieved and benefit wanes.
eCoin Pretibial Implant
At the time of this writing, there is currently only one FDA-approved option that combines the best facets of the above procedures as an in-office 10-20 minute procedure. The device is known as eCoin, and it is a nickel-sized combined battery and small computer that is placed near the tibial nerve similar in location to PTNS. However, instead of the patient returning often to keep the efficacy of PTNS, the device itself automatically stimulates the nerves that are responsible for inhibiting unwanted bladder contractions. This has the dual advantage of being a small, in-office once and done procedure, but also can stimulate and control the bladder at more regular intervals without having the patient return to the clinic. The first generation of devices have lasted at least 3 years, and likely the newer generation and newer stimulation protocols will extent that past 5 years. Replacing the device is also done in the office, and also takes 10-20 minutes.

https://ecoin.us/
Efficacy for PTNS, sacral neuromodulation, and eCoin have all been reported to be similar though likely sacral neuromodulation and eCoin have better efficacy overall secondary to frequency of stimulation and long-term compliance.
Risks of eCoin are minimal, and include infection of the implant and local pain. Both of these risks are rare. If there is a lot of edema, or swelling of the foot, or if there is evidence of poor blood flow or infection, the patient is not a candidate for eCoin.
Major Surgical Intervention
For patients that fail all the above, there are more invasive options available. These are reserved for only the most severe of all cases, and these patients are essentially what are colloquially known as bladder-cripple. These patients unfortunately have symptoms so severe that even doing simple daily activities are near impossible because of the constant need and urge to urinate, and often these bladder contractions can be painful. For these patients, the following options are available:
Bladder Augmentation
Bladder augmentation is a procedure where the patient’s bladder is surgically fashioned into a reservoir for urine rather than an active way to store and expel urine. Normally, the bladder fills to a point where the reflex arc allows the person to open the urinary sphincter – the muscle that controls bladder function – at the same time the bladder contracts to expel the urine through the urethra. However, with this surgery, the ability to do that diminishes to the point where the patient is no longer able to mount a bladder contraction. This is achieved usually by using a segment of the small intestine, and using that segment to patch on to a part of the bladder that has been opened along the top of the bladder. This then creates a big pouch that can hold urine, and since the small intestine has different nerves than the bladder, this segment does not contract. Although the bladder muscles can still potentially contract, the inclusion of the small intestine can make that contraction incomplete, and not able to expel urine. This requires at least some reservoir of bladder to begin with, and for some patients the bladder capacity is so small that augmentation cannot be performed. Usually this is in the setting of a neurogenic bladder, such as late uncompensated spinal cord injury.
However, once this procedure is performed, the patient needs a way to get the urine out. This requires the patient placing a catheter into the bladder intermittently (CIC) at least 4-5 times a day for the rest of his or her life. Also, as the small intestine produces mucous, the patient will occasionally need to place a catheter to place water or saline into the bladder to wash out the mucous plugs.
Risks are possible gastrointestinal damage such as injury, change in bowel habits, or malabsorption of nutrients that require supplements. This procedure can be done in both an open and robotic platform, and either carries a chance of bleeding, injury to an adjacent structure, or infection. There can also be electrolyte changes after surgery, and it is important to keep hydration high after any surgery on the bladder and bowel as dehydration is a major risk.
Cystectomy
For the most severe cases, cystectomy is an option. Cystectomy is the surgical name for removal of the bladder. Most often, this is done for bladder cancer, but it can also be done for severe bladder instability that can occur with neurogenic bladder. Removing a bladder can be done with an open or robotic platform, and the blood loss is less with a robotic approach.
Once the bladder is removed, there needs to be another way to empty the urine. This can be done with one of two basic principles, a conduit or a continent pouch. A conduit is often done using a piece of small intestine, known as an ileal conduit, and the patient would then urinate into a bag that can be attached to a drainage bag for continuous drainage, or a bag that can hold the urine while the patient is mobile until he or she gets a chance to empty it. A continent pouch can be an orthotopic neobladder, where a piece of small intestine is fashioned into a new bladder and attached in the normal anatomic location of the bladder, with an opening leading to the urinary sphincter and urethra. It can also be done as a pouch that leads out through a chimney that exits the body in a different location (e.g. the belly button), and a catheter is then used to intermittently drain the pouch. There are advantages and disadvantages to each of these approaches of reconstruction, and these procedures are most safely done in institutions that do a lot of these types of procedures as they have a lot of risks associated and a lot of follow-up care that is needed after the procedure to ensure success. The risks are similar to the ones outlined for bladder augmentation, but they are higher and the follow-up care is also more involved.
Below is a summary of the steps a patient and doctor may take as well as a table comparing secondary therapies.
Comparison of Secondary Therapies
|
Type of Therapy
|
Frequency of Treatment
|
Location of Procedure
|
Risks of Procedure
|
Area of Body Performed
|
Duration of procedure
|
|
Botox Bladder
|
Every 6 months
|
ASC or office
|
Bleeding, infection, urinary retention
|
Directly into the bladder by cystoscopy
|
5-10 min
|
|
PTNS
|
Initially every week, then every month
|
Office
|
Minimal
|
Pretibial (near the ankle)
|
Initial placement 20-30 min, then 5 min/session
|
|
Sacral Neuromodulation
|
Evaluation done in office, then implant performed. Changed 4-5 years or more
|
Office, then OR
|
Infection, pelvic pain, bleeding, injury during lead placement
|
Lower back, adjacent to spine and implant placed on upper buttock/lower spine
|
Nerve evaluation 30-40 minutes, OR placement 30-50 minutes
|
|
eCoin
|
Every 3-5 years, possibly longer
|
Office
|
Infection
|
Pretibial (near the ankle)
|
10-20 min
|
|
Therapy
|
Efficacy
|
Cost/5 years treatment
|
Ease for Patients
|
Frequency of Use
|
Potential Side Effects
|
Downtime After Intervention
|
Patient Compliance
|
Patient Satisfaction
|
|
eCoin
|
High
|
Low
|
Easy
|
Every 3-5 years
|
Minor pain at insertion
|
Minimal
|
High
|
High
|
|
Botox to the bladder
|
High
|
High
|
Moderate
|
Every 6 months
|
Urinary tract infections, urinary retention
|
Minimal
|
Low
|
Moderate
|
|
Percutaneous Tibial nerve stimulation
|
Moderate
|
Moderate
|
Easy
|
Every 4 weeks
|
Minor pain, skin irritation
|
Minimal
|
Low
|
Moderate
|
|
Sacral Neuromodulation
|
High
|
High
|
Moderate
|
Every 5 years
|
Infection, pain at implant site
|
Moderate
|
Moderate
|
High
|
|
Antimuscarinics
|
Moderate
|
Low
|
Easy
|
Daily
|
Dry mouth, constipation, possible dementia/cognitive effects
|
None
|
Low to Moderate
|
Low
|
|
Myrbetriq
|
Moderate
|
High
|
Easy
|
Daily
|
Headache, nausea, hypertension
|
None
|
Low
|
Moderate
|
|
Gemtasa
|
Moderate
|
High
|
Easy
|
Daily
|
Headache, nasal congestion
|
None
|
Low
|
Moderate
|
|
Bladder augmentation
|
High
|
High
|
Difficult
|
One time
|
Infection, difficulty emptying bladder, permanent need for intermittent catheterization
|
High
|
Low
|
Moderate
|
|
Cystectomy
|
High
|
High
|
Difficult
|
One time
|
Infection, difficulty emptying bladder, sexual dysfunction, need for reconstruction
|
High
|
Low
|
Moderate
|