The Categories of Male Infertility
When couples are having difficulty conceiving, often the medical workup looking into causes starts with the female. But approximately 20% of all couples that are trying to conceive have difficulty only because of male factors, and another 30% of the time both male and female factors play a role. So, 50% of couples have difficulty conceiving either in part or completely due to an issue with male subfertility!
What’s more alarming is that even though frequently the male side gets relegated to a secondary role when it comes to fertility, and therefore not tested or tested late in the process, issues with male fertility can be either corrected completely or improved on. This leads to the female getting put through extensive – or possible even unnecessary – testing and treatment.
Furthermore, issues with male fertility can be one of the few early chances to address health issues that can compound as one ages. It is a window of opportunity that, if taken, can lead to healthier lives later in life.
The workup for male infertility usually starts after a couple has been trying to conceive unsuccessfully for 6 months to a year, but if there are known issues that may prevent fertility the workup may start prior.
Often a semen analysis is performed at the onset of that evaluation. A semen analysis, also known as a sperm count or spermogram, is a laboratory test that evaluates various parameters of semen to assess a man's fertility. Here are some of the key parameters measured in a semen analysis and what they signify:
1. Sperm Count (Concentration):
- Significance: The number of sperm per milliliter of semen.
2. Total Sperm Count:
- Significance: The total number of sperm in the entire ejaculate.
3. Sperm Motility (Movement):
- Significance: Evaluates the percentage of sperm that are actively swimming and their ability to move forward.
4. Total Motile Count
- Significance: This is the single most important factor in determining a man’s fertility. It is a calculated number, taken from total sperm count (which is concentration x volume) x motility. Ideally this number is above 50 million, 20-50 million is still within a normal range but decreased probability, 10-20 million is on the very low end of the normal range and has an even more decreased probability, and below 10 million is unlikely to lead to natural pregnancy.
5. Sperm Morphology (Shape):
- Significance: Assesses the percentage of sperm with a normal shape, as abnormalities can affect fertility but most often times do not. More important than the actual number is the distribution. More specifically, it is more important to assess why a morphology is low rather than the number itself.
- Normal Range: Typically, a minimum of 4% normal-shaped sperm is considered normal.
6. Semen Volume:
- Significance: Measures the amount of semen produced in one ejaculation.
- Normal Range: Normal semen volume is usually between 1.5 to 6 milliliters. Below 1.0 milliliters is abnormal.
7. pH Level:
- Significance: Evaluates the acidity or alkalinity of the semen.
- Normal Range: Normal pH levels in semen typically range from 7.2 to 7.8.
9. Semen Liquification Time:
- Significance: Measures how quickly the semen changes from a gel-like consistency to a more liquid form, which is essential for sperm mobility.
- Normal Range: Normally, semen should become liquid within 20-30 minutes after ejaculation.
9. White Blood Cells (WBCs):
- Significance: Detects the presence of immune cells in semen, which may indicate infection or inflammation.
- Normal Range: Ideally, there should be very few or no white blood cells in the semen.
10. Fructose Level:
- Significance: Measures the presence of fructose, which is produced by the seminal vesicles and provides energy for sperm.
- Normal Range: The presence of fructose is typically normal in semen.
11. Viscosity (Consistency):
- Significance: Assesses the thickness or stickiness of semen, which can affect sperm mobility.
- Normal Range: Normal semen should not be excessively thick or sticky.
Find out more about the various causes of male infertility below.
Low Sperm Count - Find out what the definition of low sperm counts are, and the possible causes
No Sperm - This condition is referred to as azoospermia. Find out the possible causes of azoospermia, and the treatment options.
Normal Sperm Counts - Even though a man has a normal sperm count, there still may be an underlying issue that is leading to male factor infertility. Find out more.
Vasectomy Reversal - It is estimated that 5% of men who undergo vasectomy have regret about doing so and wish to reverse the process. Find out here what the options are.
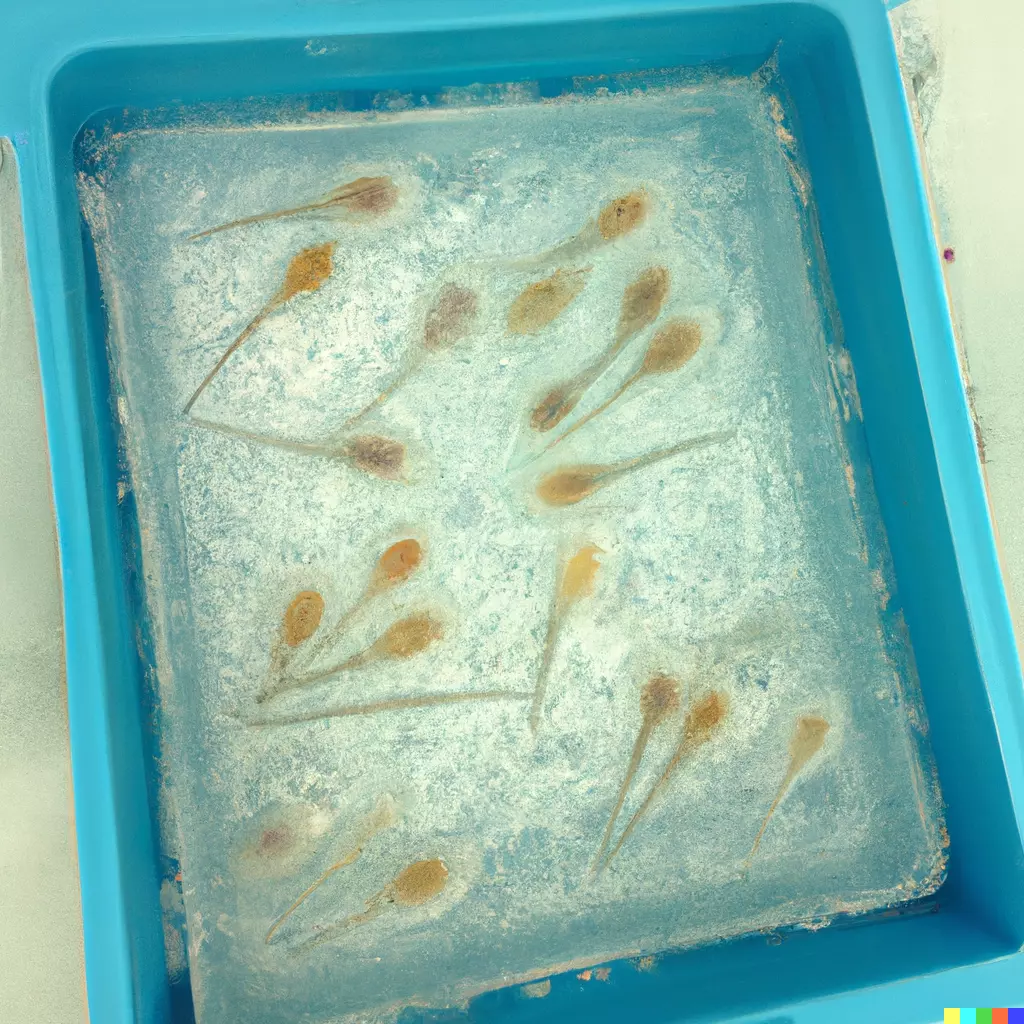
Sperm Cryopreservation - There are times when an anticipated or unanticipated event takes place (e.g. surgery, vasectomy, medical therapy, fatal illness, etc) and a couple may want to preserve sperm for future. Find out more information about sperm cryopreservation here.
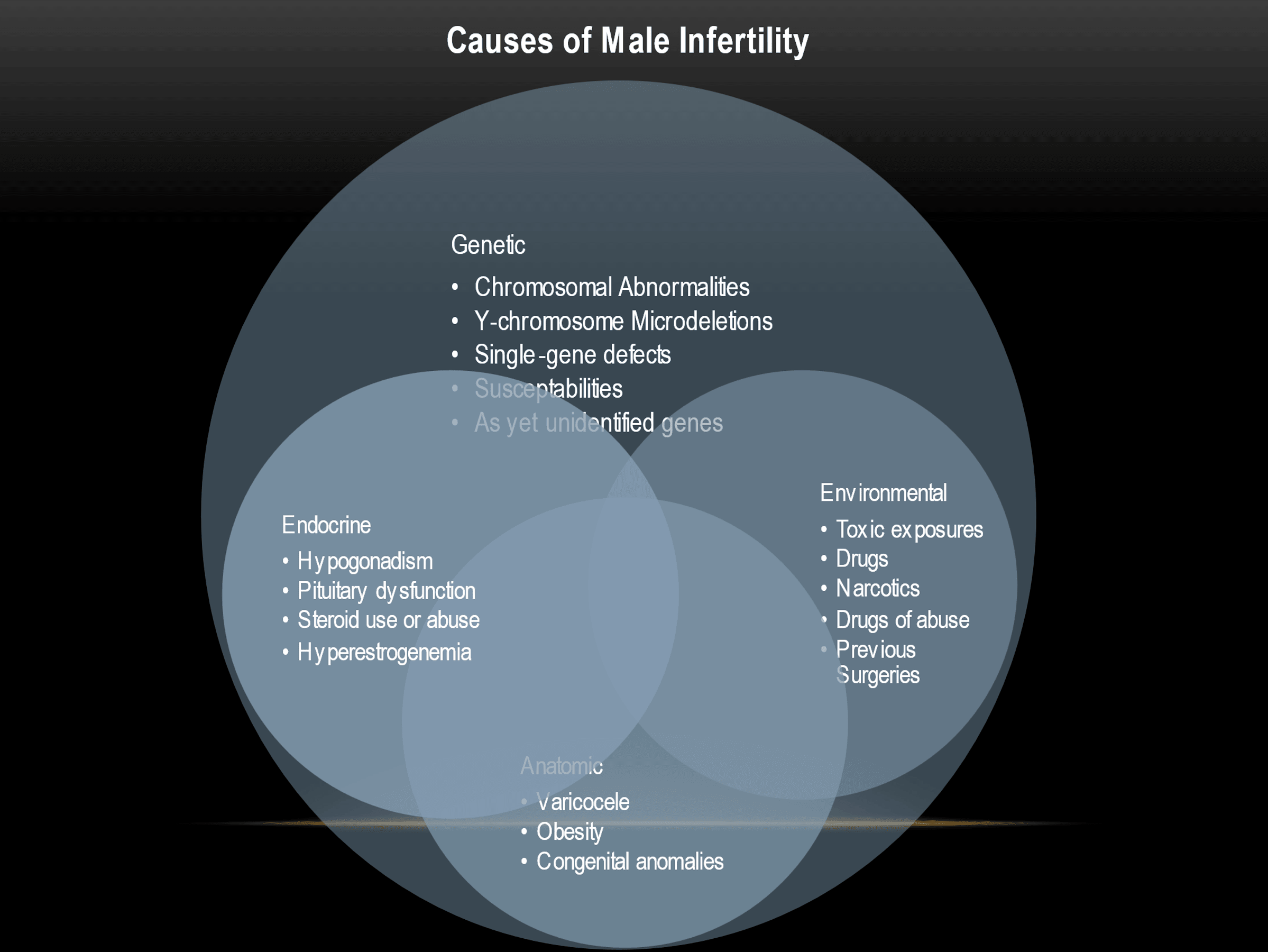
Male infertility encompasses a wide variety of potential issues. There are genetic, hormonal, environmental, and anatomic issues that can be contribute to suboptimal sperm counts.
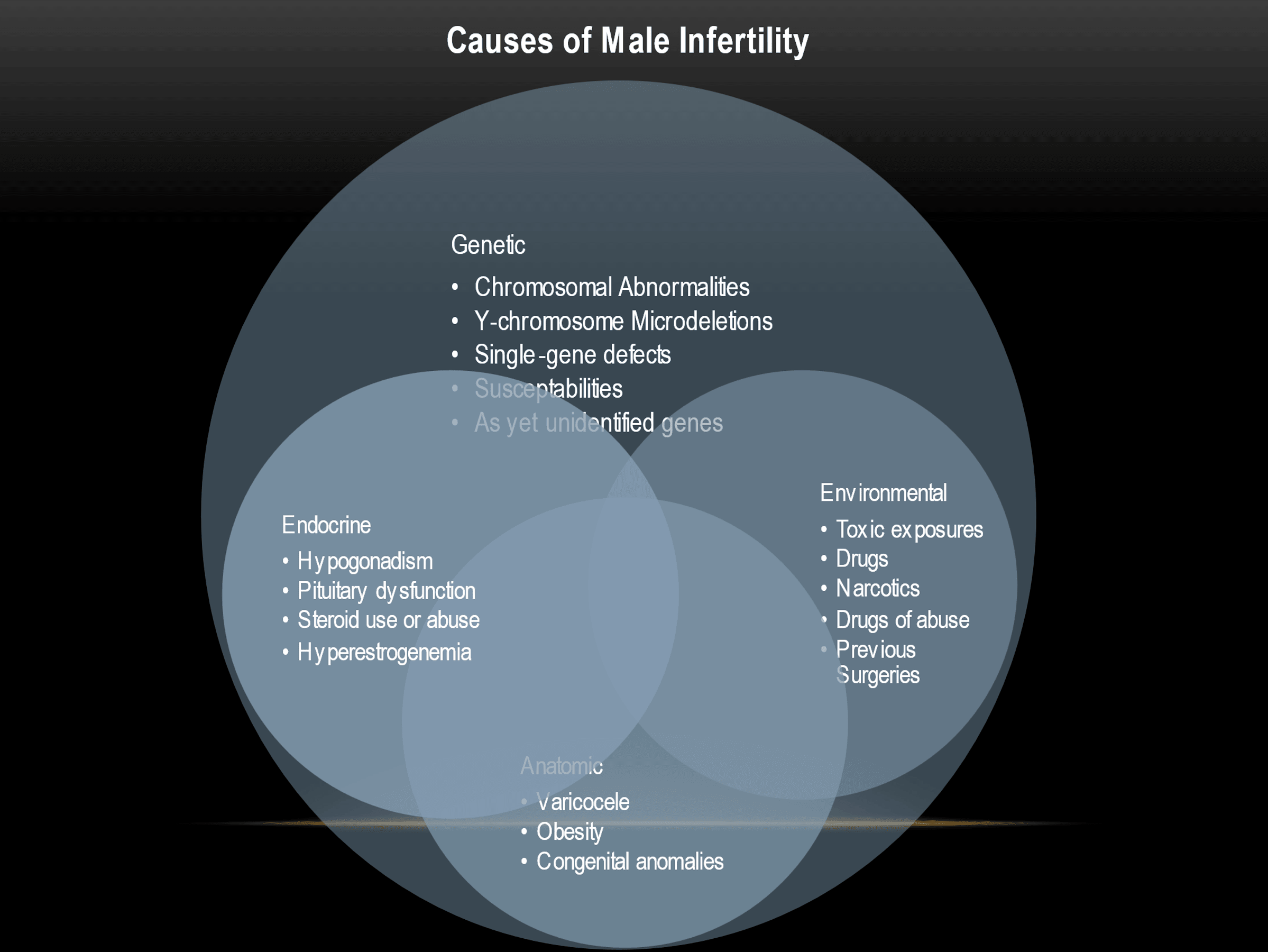
The above is not an exhaustive list. However, there are many reasons for hope if there is an issue with a man’s sperm count. Many of the above conditions can be corrected. Furthermore, even if not corrected completely, in the majority of cases a man’s sperm count can be improved, which can lead to improved outcomes.
It is important to realize that fertility involves at least two individuals, and it is important to evaluate the female counterpart, just as it is important to evaluate the male. As such, for achieving fertility, it becomes less like other forms of medicine in the sense that we deal with probabilities rather than absolutes. For example, when an individual has diabetes or hypertension, there are established reference ranges that determine those conditions. Though those reference ranges can change over time, they still represent thresholds for identifying a person as diabetic or having hypertension.
With fertility, we talk much more about probabilities. There is a probability that a male will be able to have children, and a probability that a female will be able to have children. Our goal is to increase the probability on the male side to achieve a pregnancy, and by doing so increase the overall chances of success.
Frequently Asked Questions
1. How common is male infertility?
Male infertility is relatively common, affecting about 7-10% of men worldwide. It can result from various factors, as listed below.
2. Is male infertility reversible?
Yes! Almost always, there is something that can be done, either with medications, surgical interventions, lifestyle changes or (most commonly) a combination of the above. Learn more about what can done with each specific condition below.
3. Can certain medical/health conditions contribute to male infertility?
Yes, certain medical conditions such as diabetes, hypertension, and hormonal disorders can contribute to male infertility by affecting sperm production or function.
4. How does smoking harm sperm quality and male fertility?
Smoking can harm sperm quality and male fertility by causing DNA damage to sperm cells, reducing sperm count, and impairing sperm motility.
5. Can steroid use lead to male infertility?
Steroid use, particularly anabolic steroids, can disrupt the body's hormonal balance. It may lead to decreased sperm production and potential male infertility.
6. Can stress and mental health impact male fertility treatments?
Stress and mental health issues can impact male fertility treatment by affecting hormone levels and sperm production. Managing stress and seeking mental health support can have optimistic fertility.