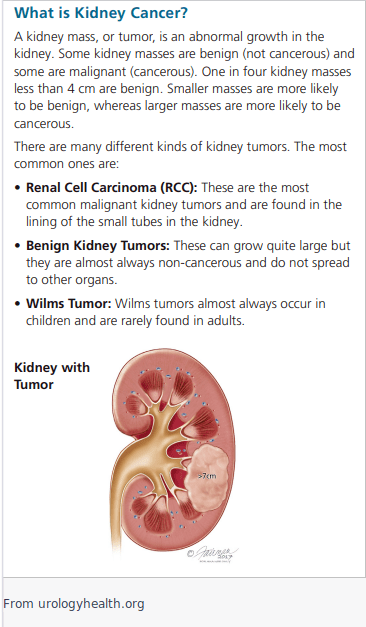
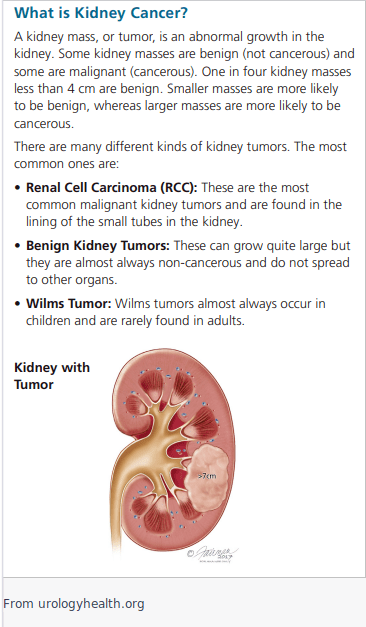
Risk factors for kidney cancer include:
-
Smoking: Smoking is a significant risk factor for developing kidney cancer.
-
Age: The risk of developing kidney cancer increases with age.
-
Gender: Men have a higher risk of developing kidney cancer than women.
-
Obesity: People who are overweight or obese have an increased risk of developing kidney cancer.
-
Family history: Having a family history of kidney cancer increases the risk of developing the disease.
-
Long-term dialysis: People who have received long-term dialysis have a higher risk of developing kidney cancer.
-
Certain genetic conditions: Certain genetic conditions, such as von Hippel-Lindau disease and hereditary papillary renal cell carcinoma, increase the risk of developing kidney cancer.
Predisposing factors for kidney cancer include:
-
High blood pressure: People with high blood pressure have a higher risk of developing kidney cancer.
-
Exposure to certain chemicals: People who have been exposed to certain chemicals, such as asbestos and trichloroethylene, have a higher risk of developing kidney cancer.
-
Kidney diseases: People with kidney diseases, such as polycystic kidney disease, have a higher risk of developing kidney cancer.
Treatment for kidney cancer may include surgery, ablation therapy, immunotherapy, targeted therapy, and chemotherapy. The most common treatment for localized kidney cancer is surgery to remove the affected kidney. The second most common treatment is known as ablative therapy, where the tumor is either frozen or burned. Some types of kidney cancer are just followed, as renal cell carcinoma can be slow growing. If the patient has many medical problems and/or is elderly and the tumor is in a site that is not easy to access, it may be more beneficial to the patient to follow the cancer rather than treat.
Surgery for kidney cancer typically involves removing the entire affected kidney (radical nephrectomy) or removing only the part of the kidney containing the cancer (partial nephrectomy). In some cases, minimally invasive laparoscopic or robot-assisted surgery may be used to treat kidney cancer. These interventions are done to remove the original source of the cancer, and in many cases this is curative. However, if there is evidence of disease outside of the kidney (known as metastatic disease), this surgery may be done before or after using medication to decrease or clear other areas of disease. This medication can also be used to shrink the cancer, making the surgery easier to perform with less risk of complications.
New medications that can be used to treat metastatic disease include:
-
Tyrosine kinase inhibitors (TKIs): TKIs are a type of targeted therapy that block the activity of certain enzymes involved in the growth and spread of kidney cancer cells. Examples of TKIs used to treat kidney cancer include sunitinib, pazopanib, and cabozantinib.
-
Immune checkpoint inhibitors: These are a type of immunotherapy that help the immune system recognize and attack cancer cells. Examples of immune checkpoint inhibitors used to treat kidney cancer include nivolumab, pembrolizumab, and avelumab.
For more information, please visit Kidney Cancer - What You Should Know - Urology Care Foundation (urologyhealth.org)
Ureter/Bladder Cancer
Bladder and ureter cancer are two different types of cancer that affect the urinary system. They are commonly known as transitional cell carcinoma (TCC) or urothelial carcinoma (UC) because the cell types of the two are the same. TCC is divided into upper tract and lower tract. UC of the upper tract (UTUC) includes the part of the kidney that attaches to the rest of the urinary tract where urine collects, known as the renal pelvis, and the ureter, which is the tube that connects the kidney to the bladder. Lower tract urothelial cancer (LTUC) is more commonly known as bladder cancer, though there are rarely types of bladder cancer that are not of this cell type. The bladder is a muscular sac located in the lower abdomen that stores urine until it is ready to be eliminated from the body, while the ureter is a narrow tube that carries urine from the kidney to the bladder. Despite the difference in their functions, bladder and ureter cancer are similar in that they both can arise from the same cell type and cause similar symptoms.
Risk Factors for TCC
The following are some of the known risk factors and causes of TCC:
-
Smoking: Smoking is a major risk factor for TCC, particularly for bladder cancer. The chemicals in tobacco smoke can damage the DNA in cells and increase the risk of cancer.
-
Exposure to certain chemicals: Exposure to certain chemicals, such as those used in the rubber and dye industries, can increase the risk of TCC.
-
Personal or family history of TCC: Having a personal or family history of TCC increases the risk of developing the disease.
-
Chronic bladder catheterization: Long-term use of a bladder catheter can increase the risk of TCC.
-
Previous treatment for bladder cancer: People who have had treatment for bladder cancer are at increased risk of developing TCC.
-
Arsenic exposure: Exposure to arsenic, either through contaminated water or other sources, has been linked to an increased risk of TCC.
-
Age: The risk of TCC increases with age, and most cases are diagnosed in people over the age of 60.
Screening for TCC
The detection of TCC usually starts with finding blood in the urine known as hematuria. This can be either from routine screening with a urinalysis by a primary care provider and referral to a Urologist (microhematuria, or blood that is not visible by the naked eye), or by seeing blood in the urine and referral or direct self-referral to a Urologist. In rare cases, the bleeding is so severe that the patient is in the emergency room, and a Urologist is called to make the diagnosis and treat. Most often, all of the above is painless, though patients can experience recurrent urinary tract infections or frequent urination that can be a result of the side effects from the cancer growing. The following is a general outline of the screening and diagnosis process for TCC:
Screening:
-
Routine screening for TCC is typically recommended for individuals at higher risk of developing bladder cancer, such as those who smoke, have a family history of bladder cancer, or have been exposed to certain chemicals.
-
The most common screening tests for TCC are urine tests, including urinary cytology (examination of urine cells) and urine tumor marker tests.
-
In some cases, other imaging tests, such as CT scans or MRI scans, may be used to screen for TCC.
Diagnosis:
-
If the screening tests suggest the presence of TCC, a diagnostic evaluation is typically performed to confirm the diagnosis and determine the stage of the disease.
-
The diagnostic evaluation typically includes a cystoscopy (visual exam of the bladder using a scope), biopsy (removal of tissue for examination), and imaging tests, such as CT scans or MRI scans.
-
In some cases, other tests, such as a ureteroscopy (visual exam of the ureter using a scope) may be used to diagnose TCC.
It is important to note that the screening and diagnosis process for TCC can vary based on the individual case, and that this outline is intended only as a general guide.
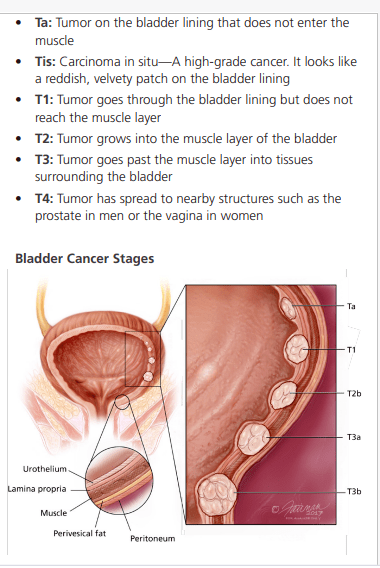
Grading and Staging of Bladder and Ureteral Cancer
The grading of bladder and ureteral cancer is determined by the appearance of the cancer cells under a microscope. Low-grade cancer cells look more like normal cells and are less likely to spread, while high-grade cancer cells are more abnormal in appearance and are more likely to spread.
Staging is used to describe the extent of the cancer, and includes information about the size of the tumor, whether it has invaded surrounding tissue, and whether it has spread to other parts of the body.
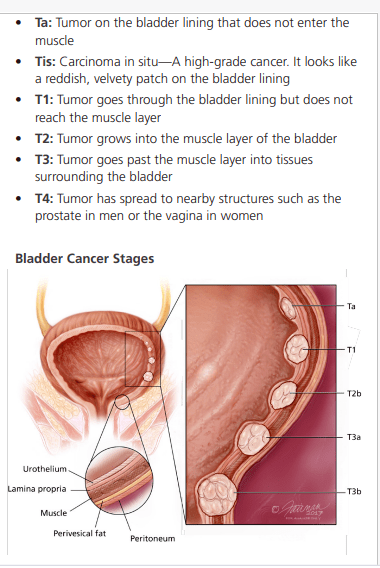
Bladder Cancer
The treatments for bladder and ureteral cancer depend on the grade and stage of the cancer, as well as the overall health of the patient. Some common treatments for both bladder and ureteral cancer include surgery, chemotherapy, and radiation therapy. Bladder cancer is far more common than ureteral cancer.
For low-grade bladder cancer, a transurethral resection of the bladder tumor (TURBT) may be recommended, which involves removing the cancerous tissue through a scope inserted through the urethra. If the cancer has not spread beyond the bladder, TURBT may be curative.
Bladder cancer is usually diagnosed based on the stage of the disease, which refers to the extent of the cancer and how far it has spread. The following is a general outline of the diagnosis and treatment algorithm for bladder cancer based on the stages of carcinoma in situ (CIS), Ta, T1, and T2 or higher:
Carcinoma in situ (CIS):
-
Diagnosis: CIS is diagnosed through a combination of cystoscopy (a visual exam of the bladder using a scope), biopsy (removal of tissue for examination), and imaging tests.
-
Treatment: Treatment for CIS typically involves transurethral resection of bladder tumor (TURBT) to remove the cancer cells. This may be followed by intravesical therapy (direct instillation of medication into the bladder) to reduce the risk of recurrence.
Ta:
-
Diagnosis: The diagnosis of Ta is typically made through a combination of cystoscopy, biopsy, and imaging tests.
-
Treatment: Treatment for Ta typically involves TURBT, followed by intravesical therapy based on grade. In some cases, additional treatments, such as radiation therapy or partial cystectomy (removal of part of the bladder), may be recommended.
T1:
-
Diagnosis: The diagnosis of T1 is typically made through a combination of cystoscopy, biopsy, and imaging tests.
-
Treatment: Treatment for T1 may involve TURBT, followed by systemic therapy, partial cystectomy, or radical cystectomy (removal of the entire bladder). The choice of treatment will depend on factors such as the size and location of the tumor, the overall health of the patient, and other medical conditions.
T2 or higher:
-
Diagnosis: The diagnosis of T2 or higher is typically made through a combination of cystoscopy, biopsy, and imaging tests.
-
Treatment: Treatment for T2 or higher usually involves radical cystectomy, often with the addition of systemic therapy, radiation therapy, or both. In some cases, nerve-sparing cystectomy may be performed to preserve bladder function. In rare cases, a partial cystectomy may be performed, though this may increase the risk of recurrence (the cancer coming back at the site or at a different site).
For high-grade bladder cancer, a radical cystectomy, which involves removal of the entire bladder, may be recommended. In some cases, a urinary diversion procedure may also be performed to create a new way for urine to leave the body.
For more information, please visit Bladder Cancer Patient Guide - Urology Care Foundation (urologyhealth.org)
Upper tract urothelial cancer
Grading: The grading of UTUC is based on the appearance of the cancer cells under a microscope and helps to predict how the cancer will behave and respond to treatment. UTUC is used to be graded on a scale of 1 to 3, with grade 1 being the least aggressive and grade 3 being the most aggressive. However, now more commonly it is simply graded as high grade or low grade.
Staging: The staging of UTUC is used to determine the extent of the cancer and helps to guide treatment decisions. Staging is based on the size and location of the tumor, whether it has invaded nearby tissues or organs, and whether it has spread to other parts of the body. UTUC is usually staged using the TNM system, which stands for Tumor, Nodes, and Metastasis.
Treatments for UTUC vary based on the grade and stage of the cancer, as well as the overall health of the patient. Surgery is the most common treatment for UTUC, and may include removal of part or all of the affected
kidney or ureter. The type of surgery will depend on the size and location of the cancer, the grade of the cancer, as well as the overall health of the patient. Newer treatments such as Jelmyto can be employed to treat low grade UTUC in some cases, and save the patient from more invasive surgeries, In some cases, radiation therapy, chemotherapy, or a combination of both may also be recommended.
For more information, please visit Upper Urinary Tract Cancer: Symptoms, Diagnosis & Treatment - Urology Care Foundation (urologyhealth.org)
Prostate cancer
Prostate cancer is a common type of cancer in men, and early detection and treatment are key to improving the chances of a successful outcome. Early detection typically relies on a physical examination, known as a digital rectal exam (DRE) and PSA. Please follow the link for more information on PSA and PSA screening as well as prostate biopsy [link to elevated PSA].
Confirmation of prostate cancer is made on biopsy, and staging is done based on biopsy results as well as imaging (MRI, bone scan, CT/PET scan, or a combination of the above).
The following is an overview of the treatment options for prostate cancer:
Active Surveillance:
-
Active surveillance is often recommended for men with slow-growing, low-risk prostate cancer.
-
This involves regular monitoring of the cancer through PSA tests, prostate biopsies, molecular and genetic tests, and other imaging tests, without immediate treatment.
-
Treatment is typically initiated if the cancer begins to grow or spreads beyond the prostate.
Surgery:
-
Radical prostatectomy (removal of the entire prostate gland) is the most common type of prostatectomy, and can be performed using various techniques, including nerve-sparing techniques to preserve bladder and sexual function.
-
Robotic-assisted prostatectomy are minimally invasive techniques that can offer faster recovery times and fewer complications than open prostatectomy.
Radiation Therapy:
-
Radiation therapy, including external beam radiation therapy and brachytherapy (internal radiation therapy), can be used to treat prostate cancer.
-
Radiation therapy can be used as the primary treatment for prostate cancer or in combination with other treatments, such as surgery or hormonal therapy.
Hormonal Therapy:
-
Hormonal therapy, also known as androgen deprivation therapy, works by reducing the levels of male hormones (androgens) that fuel the growth of prostate cancer.
-
Hormonal therapy can be used as the primary treatment for prostate cancer or in combination with other treatments, such as radiation therapy or surgery.
Chemotherapy:
Minimally invasive treatments for localized prostate cancer have been developed in recent years to offer alternatives to traditional surgical or radiation therapy. These treatments aim to preserve quality of life and reduce side effects while effectively treating the cancer.
Ablative therapies include high-intensity focused ultrasound (HIFU) and cryotherapy, which use heat or cold to destroy cancerous tissue. HIFU uses high-frequency sound waves to heat the prostate tissue, while cryotherapy uses extremely cold temperatures to freeze and destroy cancerous tissue.
Focal treatment of prostate cancer is a technique that targets only the area of the prostate where the cancer is located, rather than treating the entire gland. This can be done using techniques such as focal laser ablation, focal high-intensity focused ultrasound (HIFU), or focal cryotherapy. These techniques are intended to be less invasive than treating the whole gland and to preserve surrounding healthy tissue.
These minimally invasive treatments are still considered to be relatively new, and more research is needed to fully understand their efficacy and long-term outcomes. However, initial results are promising and they are becoming more widely available to patients as options for the treatment of localized prostate cancer. It is important to understand that these therapies are not good options for many men with more aggressive or advanced disease, and most are not covered by insurances as their long-term efficacy data is not established (how effective they are at treating the cancer over the long term).
For more information about Prostate Cancer Treatment, please use the following link: Educational-Resources - Urology Care Foundation (urologyhealth.org)