It is important to note that this is a subjective process – like art, it is dependent on who is looking at the sample. This is different than other forms of testing. For example, when a blood test is done, there is a fairly accurate number that is more reproducible than either a computer or a person making interpretations of what they see through a microscope. This means that there is some expected variation, and therefore the first take home point is that one should always do a semen analysis at a reputable lab, that has done many of them.
However, of all the above data points, the one that has been shown to correlate the best with a man’s fertility potential is known as the total motile count. This refers to the total number of motile – or “wiggling” – sperm that a man has. It is the best indicator we have of a man’s fertility potential. Sometimes it is listed in a semen analysis, and sometimes it is simply calculated based on the information that is provided. To calculate a semen analysis, the following equation is used:
Total motile count (TMC) = volume (in milliliters or mL) x concentration (in millions of sperm/mL) x motility (as a percentage or %)
It is important to remember that this represents ranges, rather than rigid numbers, as sperm counts themselves are subject to a high amount of variation. But just as a general reference range:
|
Total Motile Count (TMC in millions of sperm)
|
Available options for a successful pregnancy
|
Comments
|
|
0-1 million
|
In-vitro fertilization (IVF) is the only option
|
This is often referred to as cryptozoospermia, or a few sperm reported on a semen analysis. * IVF recommended, oftentimes with testicular sperm extraction (TESE)
|
|
1-5 million
|
IVF (but often TESE not needed)
|
Sometimes TESE is performed in this population if there is a suspicion that the ejaculated sperm has accumulated many defects
|
|
5-10 Million
|
Intrauterine Insemination (IUI) is an option, as well as IVF
|
IUI is a procedure where sperm is washed, and injected into the cervix for assisted reproduction during wither a natural or endocrine-augmented ovulation cycle
|
|
10-20 million
|
IUI, low chance of natural pregnancy
|
Although this marks the beginning of normal sperm counts by World Health Organization criteria, and there is a percentage of men that will conceive naturally with these counts, the probabilities are still lower
|
|
20-50 million sperm
|
IUI, moderate chance of natural pregnancy
|
Probabilities of natural pregnancy start to rise to near normal levels
|
|
Above 50 million sperm
|
Natural pregnancy
|
Sperm is optimized for pregnancy
|
* For cryptozoospermia, often a semen analysis will have a comment written referring to only a few motile, nonmotile, or a few motile and nonmotile sperm. This is not all the sperm in the ejaculate. For example, a report that states 2 motile and 3 nonmotile sperm does not mean there is 5 total sperm in the ejaculate, but rather seen on the small grid under the microscope that is being extrapolated to the whole specimen, which would correlate to anywhere from 200-500,000 sperm for example.
It is important to remember that though the above numbers represent reference ranges, and our best way of predicting a man’s reproductive success, it is still inexact. Studies have shown up to 20% of couples presenting to fertility clinics with inability to conceive will have difficulty because of the male component, but total motile counts are normal. There are other considerations that a semen analysis considers, and even if those factors are normal there can be an issue with the DNA within the sperm, rather than the sperm itself. Please click here to review other factors that can impact sperm and fertility:
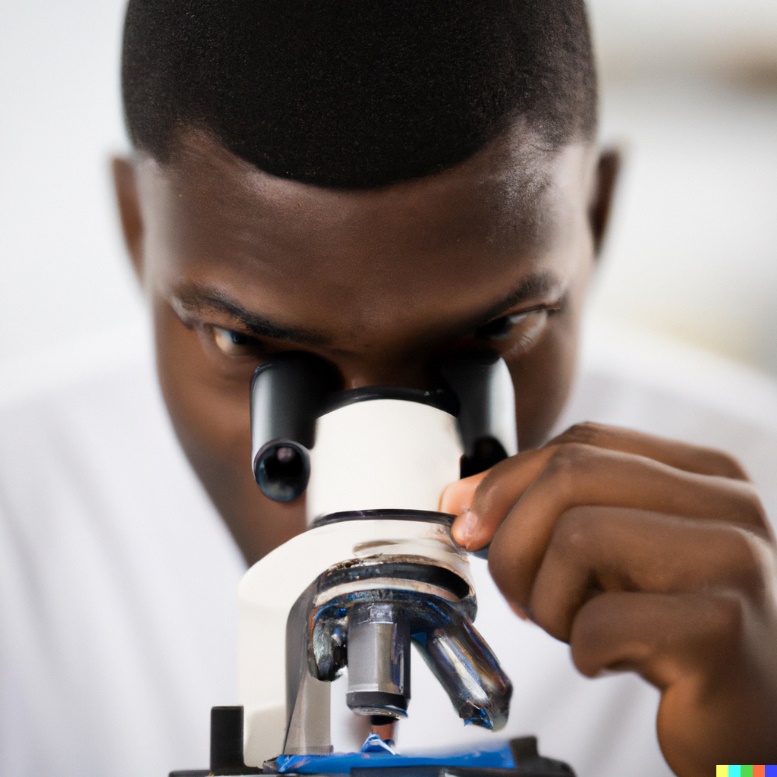
In general, an issue with a man’s fertility potential can be classified into one of four broad categories that are not mutually exclusive (meaning one of these categories can influence the others). These broad categories are hormonal, genetic, environmental, and anatomic issues that can affect fertility.
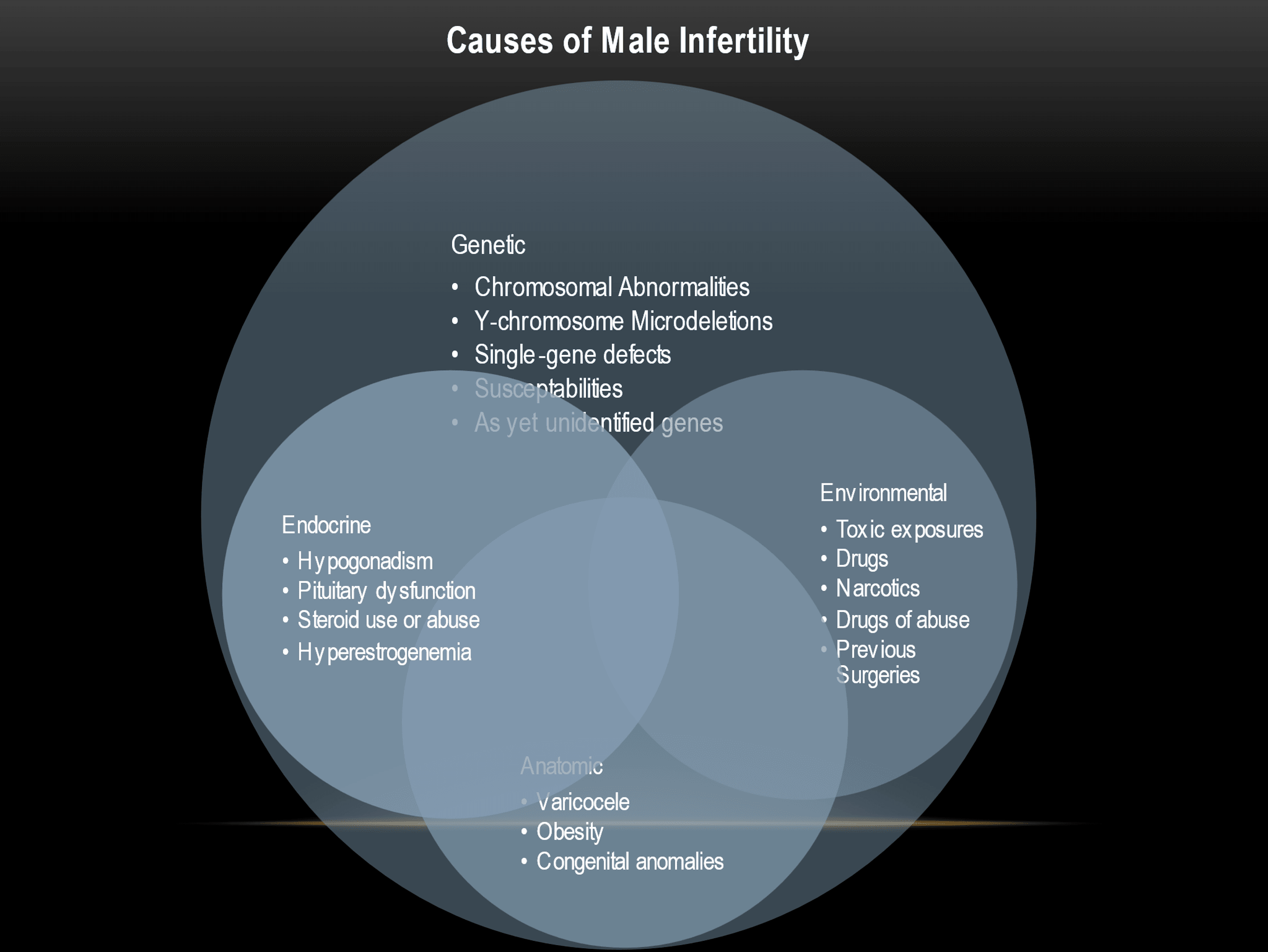
In general, these represent examples and are not meant to be an exhaustive list. To go over these categories in more detail, see below.
Genetic
Genetics can influence almost all aspects of male infertility. To some degree, our genetics play a role in almost all aspects of life, though the degree that our genetic makeup influences any specific aspect of life varies greatly. It is no different for fertility, where genetics can influence a man’s fertility potential, but to varying degrees based on the male. For some, genetic aberrations can be the sole cause of a man’s infertility, and for others genetics play only a very minor role in the reason behind an inherent fertility issues.
The other complicating factor when it comes to genetics is that though our knowledge of genetics expands exponentially daily, we are still not at the point as a medical society to determine all the genetic influences that can affect a male’s fertility potential. Furthermore, we are not medically or ethically at the point where a doctor can alter a man’s genetics to aid fertility potential.
As such, the group we focus on for doing a genetic evaluation primarily relates to men with no sperm (a condition we refer to as azoospermia), or on occasion next to no sperm (the cryptozoospermia category from above), as the question with these men is if it is even possible to have children.
Please click on the link below to find out more about the genetic testing and causes of azoospermia
[No Sperm]
So long as a man has even a little sperm, we know it is at least possible for that man to have children with assisted reproduction, it is just a matter of what we can do to help to achieve that goal.
Hormonal
A hormone refers to a regulatory substance produced in the body and transported in tissue fluids to another part of the body or even within the same organ. Hormones influence many different aspects of health, and in the reproductive system the play a vital role when it comes to sperm production.
Although over 50 different hormones or hormone subtypes have been implicated in playing a role in male reproduction, the primary hormone that has been associated with sperm growth and maturation is testosterone. Testosterone is primarily produced in the testis in males. It slowly diffuses to the rest of the body, but within the testes the concentration of testosterone is 40-100 times that in the rest of the body. The reason it is so concentrated is because for sperm to grow and divide, it is essential that sperm be bathed in high levels of testosterone.
Thus, we do a morning testosterone test as a window into what is going on in the testes at any given time. We also account for various proteins that can influence that testosterone to calculate a true, or bioavailable, testosterone that can be a more accurate window into the testosterone status in the testes.
We also calculate pituitary hormones that can influence testosterone levels. The pituitary gland is often referred to as the “master gland” in the body and influences many different hormonal systems, including testosterone levels. The pituitary gland also influences thyroid levels, which can play a small role in sperm production. Finally, there can be an overproduction of a hormone called prolactin, which can adversely affect both testosterone and sperm counts. Depending on a man’s symptoms, it becomes important to check these potential hormonal influences on sperm counts.
Finally, we also check estradiol levels. All men have a little bit of estrogen, just like all women have a little bit of testosterone. Testosterone is converted into estradiol by an enzyme called aromatase, a component of different types of cells in the body but is found in higher quantities in fat cells. This is one of many reasons obesity can contribute to a decrease in sperm counts. Although as an absolute value the amount of these estrogens can be low relative to the female body, relative to testosterone if these values are high, it can have an adverse effect in the production of both testosterone and sperm.
Anatomic
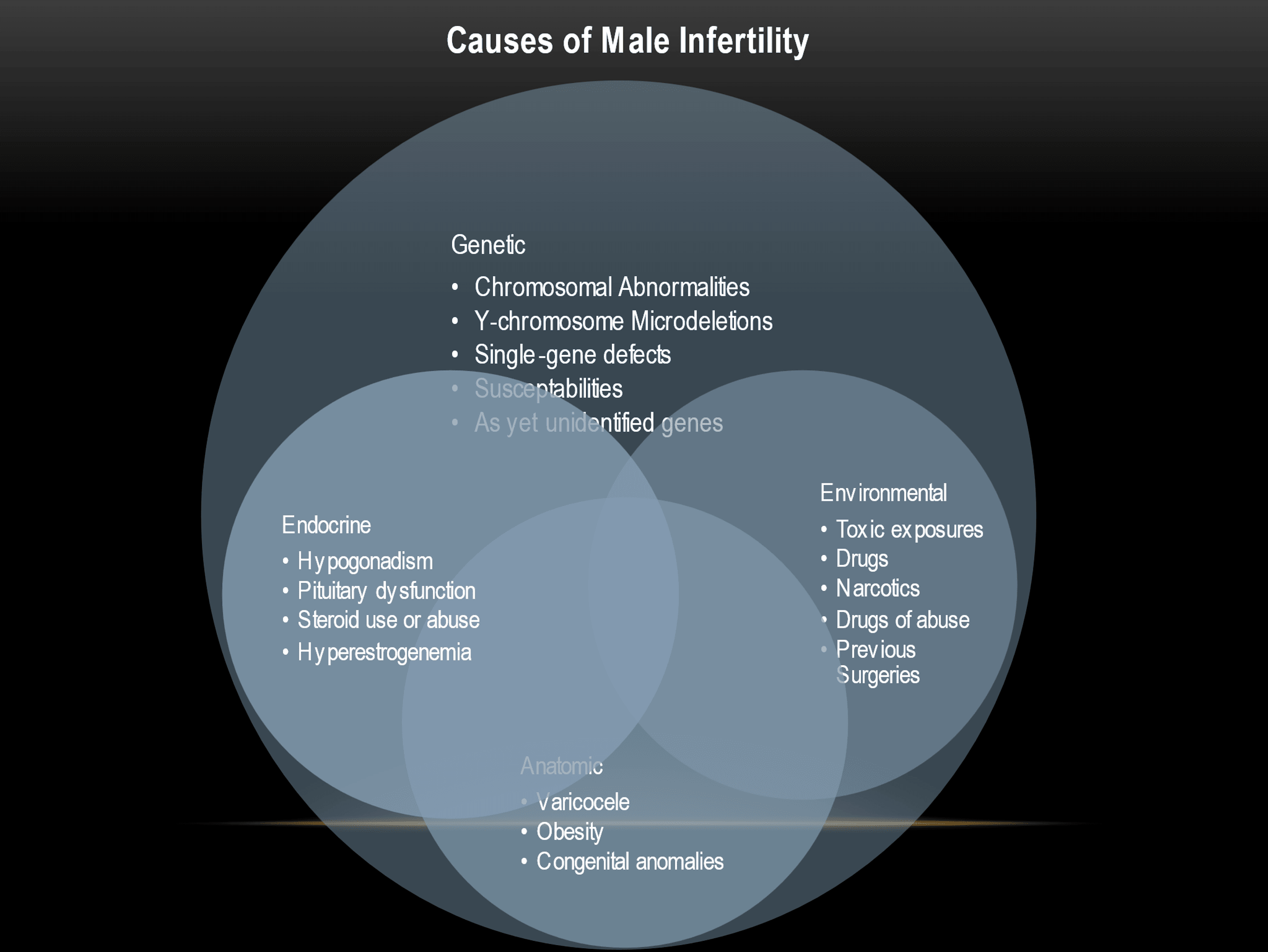
There are many physical characteristics that can influence a man’s fertility potential. Many of these influences are secondary to optimal temperature considerations in the testes. For a visual reference of male anatomy, please reference the link below, this can also be used to take to your urologist to make notes.
Reproductive Basics - Urology Care Foundation (urologyhealth.org)
A man’s scrotal sac is designed to be 3-5 degrees F cooler than the rest of the body to have optimal sperm growth and maturation. There are various conditions that can influence this. Some of the more common ones are listed below. Although this is not an exhaustive list, it does highlight some of the more common anatomical reasons for lower sperm counts.
Obesity: A significant increase in fat content in and around the scrotal sac can cause an insulating effect around the testes. This insulating effect can make it difficult for heat to dissipate, in essence heating the area around the scrotum and the testes inside of it.
Retractile or inguinal testes: During development, the testes have two phases in which to be in the proper location. The first occurs in utero, when the testes first descend into the scrotal sac. A failure at birth of the testis to descend to the scrotal sac may require a surgery to be performed to place the testis in the scrotal sac within the first year after birth. If this surgery, sometimes known as an orchidopexy and sometimes done in conjunction with a surgery for a hernia repair as a one or two step procedure, is not done or done too late then there can be longstanding effects on sperm counts after puberty. Sometimes the testes can fail to descend at all, a condition known as cryptorchidism. If this occurs, there is little chance of these testes producing viable sperm in the future.
The second time descent of the testes occurs is during puberty, where the testes descend further into the scrotal sac and start to fully mature. If this process is stunted, or if the testes retract higher into the scrotal sac and must be manually pulled into the scrotal sac, this can also lead to problems with sperm growth and maturation.
Varicocele: The veins in our bodies operate on a low-pressure system. As such, to make sure blood flows back into the heart, our bodies have valves in our veins so that blood flows in a one-way direction.
However, during puberty, the testes descend and with that those veins that bring blood away from the testes descend as well. This can stretch those valves in the veins to the point that they don’t stop backflow of blood back to the testes. This can then lead to a heat sink effect, where that pooling of blood around the testes can heat up the testicle, and lead to decreases in sperm parameters. This is more common to occur on the left testicle as it is on the right, as the way the veins come back into the body is different on either side. It is also important to note that varicoceles, especially a left-sided varicocele, are very common, and presence of a varicocele does not automatically mean there is an issue with sperm counts or that it is the reason for a low sperm count.
For more information about varicoceles, please download the AUA information page about varicoceles located here: https://www.urologyhealth.org/educational-resources/varicoceles
Other anatomic factors to consider are ones that can contribute to a low volume of ejaculate, no ejaculate, or white blood cells in the ejaculate that may contribute to low sperm counts.
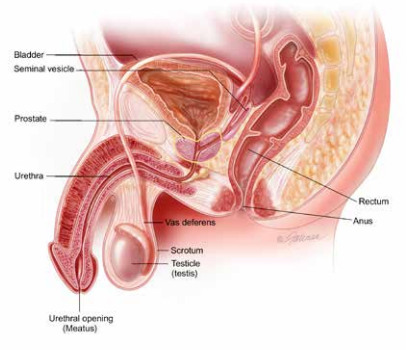
Male Reproductive Tract, from the AUA/urologyhealth.org
Low volume ejaculate: A normal semen volume is determined to be greater than 1.5 ml of ejaculate, 1.0-1.5 ml is considered borderline low, below 1.0 ml is considered abnormal or a low volume ejaculate. Some men have no ejaculate volume at all, though orgasm is still present, a condition known as anejaculation. It is important to know a little about male anatomy, as shown above, that can be useful to show why a man can have a low volume ejaculate. Many physicians also do not realize that only about 1-2 % of a man’s ejaculate volume comes from sperm. About 30% comes from the prostate, and about 60% comes from the seminal vesicles. The two combine with sperm in the ejaculatory duct, and get expulsed through an exit from the prostate into the prostatic urethra. During the contraction of these structures, a muscle known as the internal sphincter (a circular muscle) located between the prostate and bladder contracts a split second before the ejaculate comes out, ensuring the semen flows through the penis and not back into the bladder. A low volume of ejaculate can be due to multiple causes, but basically are divided into two categories.
-
Retrograde ejaculation: Retrograde ejaculation is when some or all the ejaculate passes in the direction of the bladder rather than out the penis through the urethral opening. This can be due to a malfunctioning internal sphincter, or because of previous surgery that may have removed part or all of that sphincter. Various conditions that may cause this including diabetes, certain medications such as medications for the prostate (though these are more likely to cause hypo- or anejaculation), previous pelvic surgery, previous prostate surgery, spinal injury or disease, and certain neurologic diseases. Anejaculation can also occur from certain blood pressure medications (e.g. thiazides, phentolamine) antipsychotic medications (e.g. haloperidol, chlordiazepoxide), or certain antidepressants (e.g. imipramine, amitriptyline).
-
Ejaculatory duct obstruction: The ejaculatory duct, as highlighted in the picture above, is the conduit for most of the material that eventually constitutes semen. It combines seminal vesicle contents (about 60% of ejaculate), and sperm from the vas deferens (about 1-2% of ejaculate). It travels through the prostate, which then contributes another 30% to the total semen volume. When this conduit is obstructed, it can lead to a lower volume of ejaculate. Note that this is different than when the vas deferens is obstructed, in which case semen volume is only 1-2% decreased and therefore appearing normal in volume. Examples of reasons this conduit can be blocked are because of scar tissue from infection, previous surgery or damage to the urethra, stones that can form in the prostate, or a man may have been born with a reason for blockage (known as congenital reasons). Examples of congenital reasons are a prostatic cyst, or a narrowing or malformation of the ejaculatory duct and adjacent structures from conditions such as a mutation in the cystic fibrosis gene.
Environmental
Sperm counts are very sensitive to external and internal changes in the body. There is an ever-growing list of influences, from the food we eat to the diseases we endure to even the places we live, that can influence sperm counts.
To detail every single influence on sperm counts would likely take an encyclopedia’s worth of information. Some of the more common influences on sperm counts however are briefly discussed here.
Immunologic: Immunologic infertility in males is a type of male infertility that occurs when the immune system produces antibodies that target and attack the sperm cells. This can lead to reduced sperm counts, impaired sperm quality, and ultimately, infertility.
Normally, the immune system is designed to recognize and attack foreign invaders, such as viruses and bacteria, while leaving the body's own cells and tissues alone. However, in some cases, the immune system may mistakenly identify the sperm cells as foreign invaders and produce antibodies to attack them.
Antibodies are proteins that are produced by the immune system in response to foreign invaders. In the context of immunologic infertility, antibodies may bind to the sperm cells and impair their function in several ways. For example, antibodies may prevent the sperm cells from properly binding to and penetrating the egg during fertilization. Antibodies may also cause damage to the sperm cell membrane or interfere with the normal biochemical processes involved in sperm production and function.
Immunologic infertility can interfere with sperm function in several ways. In addition to impairing the sperm cells themselves, antibodies may also cause inflammation and damage to the reproductive tract, including the testes, epididymis, and prostate gland. This can lead to a reduction in sperm quality and quantity, as well as impaired sperm motility and function.
The causes of immunologic infertility in males are not fully understood, but it may be associated with a variety of factors, including infections, injury, surgery, and certain medications. In some cases, immunologic infertility may be related to an underlying autoimmune disorder, in which the immune system mistakenly attacks the body's own cells and tissues.
Treatment options for immunologic infertility depend on the underlying cause of the condition. In some cases, treatment may involve the use of medications to suppress the immune system and reduce the production of antibodies. In other cases, techniques such as intrauterine insemination (IUI) or in vitro fertilization (IVF) may be used to bypass the effects of the antibodies and achieve pregnancy.
Acute changes in health: It is common for sperm counts to drop temporarily after an acute change in health. This can be due to a surgery (not necessarily one in the genital region), an infectious disease such as COVID-19 or the seasonal flu, or a sudden prolonged increase in activity or exposure to a heated environment. These changes are usually temporary however, and usually resolve after 3 months. It is important to remember that it is common for sperm counts to cycle to, and the frequency of that cycle can affect a given sperm count at any point in time. As an example, a man’s sperm count is different 2 days from now as it is 4 days from now, it is normal do have 2-3 day variations as well as 4-6 month cycle variations. However, a large sudden drop can occur from one of the above reasons, and if this happens it is not uncommon for sperm to require 3 months or more to recover to previous levels.
Hot Baths and Saunas: Testicular temperature plays a vital role in sperm growth and maturation. As such, exposing testes to continuous elevations in temperature, such as those environments found in hot tubs or saunas, can potentially decrease sperm counts. It is important to note these changes may happen with these activities when they are a habit – in other words, once or twice a year will likely not meaningfully change sperm counts, but every other day might. Also, less impactful activities such as a daily hot shower, are unlikely to adversely affect sperm counts.
Smoking: Smoking can adversely affect sperm counts. The reasons for this are many, from the toxins found inside of smoke when inhaled as well as the potential decreases in small vessel blood flow that can cause scarring within the testes. This seems to be both time and dose dependent, so decreasing the frequency and amount of smoking can have beneficial effects in terms of sperm counts.
Medications: Some medications may decrease sperm counts, while others are unlikely to affect sperm counts at all. The list of medications that can affect sperm counts are exhaustive, so if you are a male attempting to conceive it is important to consult the prescribing physician and let them know that you are actively trying to have children, so that they may find an appropriate alternative medication if possible.
Marijuana/Cannabinoids: The term Cannabinoids refers to group of compounds that are or are chemically similar to active component from marijuana. These can either be grown or synthetically made. Common examples are marijuana or hashish, but can extend to synthetic analogs or distilled formulations from the cannabis plant or resin. Some more commonly recognized chemicals from the process are THC (tetrahydrocannibol), primarily responsible for the psychoactive effects associated with marijuana, and CBD (cannabidiol), which does not have psychoactive effects and is actively researched for its potential health benefits for a variety of conditions.
Research into the effects of these medications on sperm production primarily fall into two categories, one into the role of cannabinoid receptors within testicular tissue and the second are effects these medications can have on sex hormone receptors. There is compelling evidence that both pathways can be negatively affected by consuming or intake of cannabinoids in most forms. While there is still a lot of research to be done, and dose-dependent use of marijuana does not affect all males the same way, it is also clear cannabinoids can affect susceptible males significantly. In other words, if there is a decrease in sperm counts, while that may not be due to cannabinoid use or consumption, it may be at least contributing to low sperm counts, if not the primary reason.
We recommend decreased use of any form of cannabinoids in whatever form if there is evidence of low sperm counts.
Testosterone use: The use of testosterone, whether in oral, injectable, or skin application forms, can and likely will decrease sperm counts. In fact, this has been used for multiple decades as a somewhat effective form of male contraception (the reason it is not yet FDA approved for such a purpose is that it is 90-97% effective depending on current formulations -- which is still low – and a small percentage of men do not recover sperm counts for years if at all).
There are also many non-prescription, over-the-counter “testosterone boosters” that area available either on the internet or at a local drug or grocery store. Some of these nutraceuticals can contain plant phytosterols, which are compounds found in plants that can mimic sex hormones. These can potentially decrease sperm counts as well, and as there is no clinical evidence for most of these nutraceuticals that they even increase testosterone levels, we do not recommend their use.
As such, before starting any form of testosterone therapy, it is imperative to let the treating physician know if you desire children in the future. There are many options for men that have low testosterone to treat in a way that can preserve, and in some cases even improve, sperm counts.
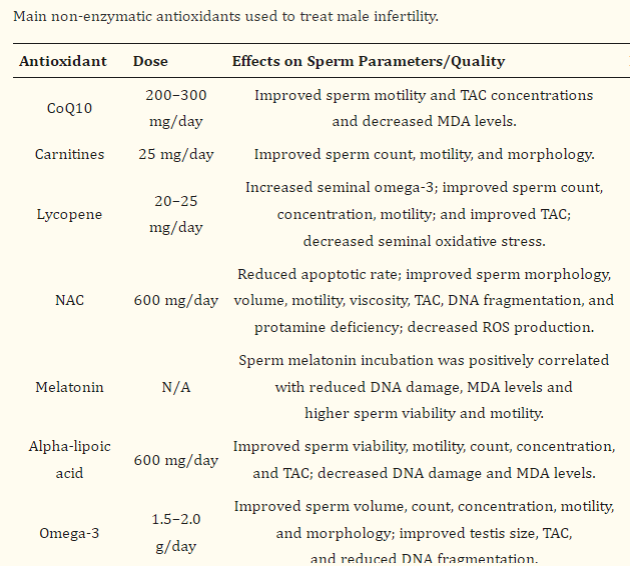
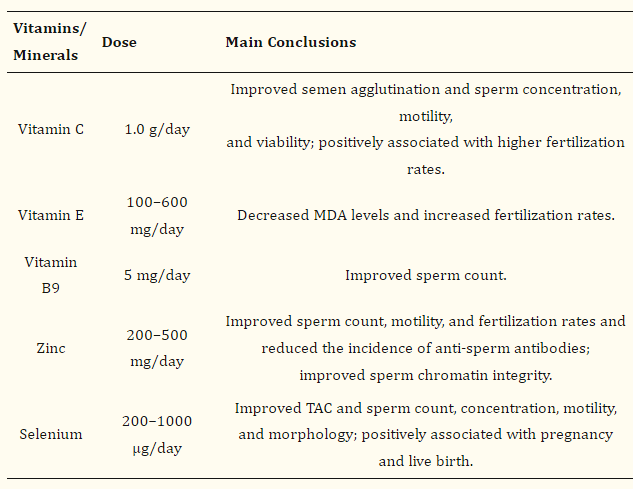
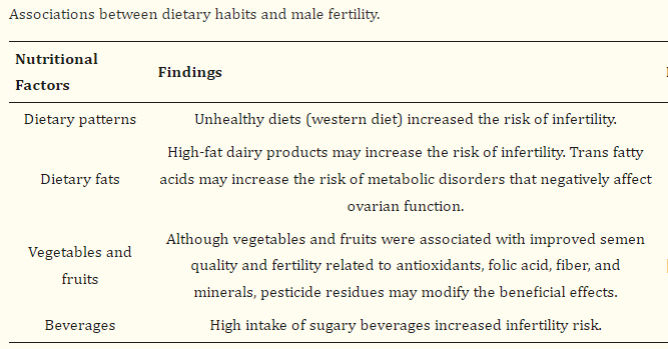
However, even if there are slight decreases in sperm counts, we advise changes to diet and activity that can help with sperm counts. Please follow the link to various diet, vitamin, and activity recommendations to help with sperm counts. Listed below is a helpful list of nutraceuticals may be helpful. Maybe the most helpful of these may be Co Q10. Coenzyme Q10 is a medication that can assist with sperm function and possibly with count. According to trials, the recommended dose is 200 mg twice a day (400 mg/day total). The liquid version of Coenzyme Q 10, otherwise known as Ubiquinone, may achieve the same result at 300 mg/day. You do not need a prescription and may obtain either at your local grocery store or pharmacy. You may also purchase Coenzyme Q10 online .
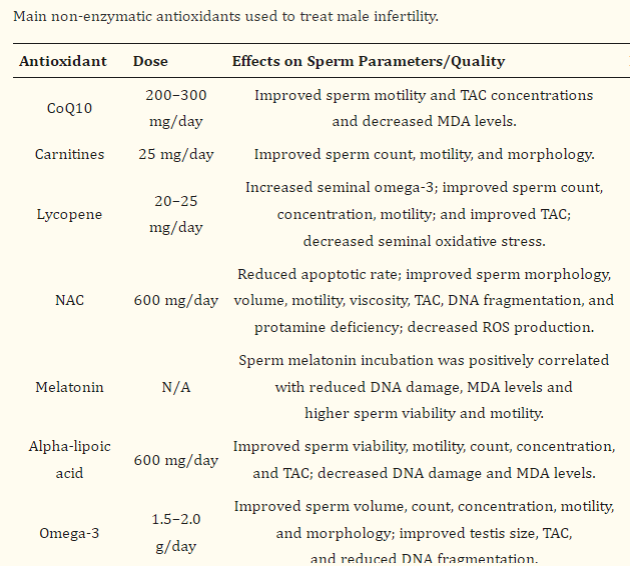
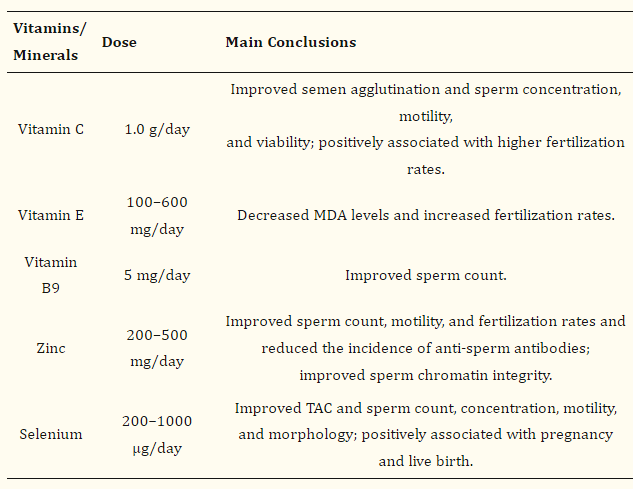
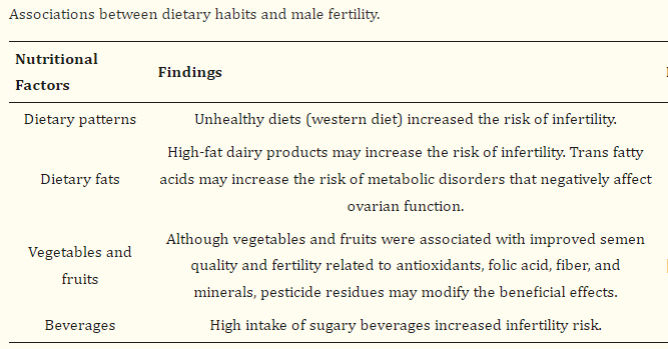
From Mourad Assidi Cells. 2022 May; 11(10): 1711.
Sleep: Sleep plays an important role in overall health and well-being, and recent research suggests that it may also have a significant impact on sperm count and fertility.
Studies have found that men who get adequate sleep have higher sperm counts and improved sperm motility compared to men who do not get enough sleep. It is believed that sleep deprivation may interfere with the body's hormonal balance, which can affect sperm production and quality.
One study found that men who slept less than 5 hours per night had a significantly lower sperm count and lower sperm motility compared to men who slept 7-8 hours per night. Another study found that men who slept for shorter periods of time had lower testosterone levels, which can impact sperm production and fertility.
Additionally, stress and anxiety, which can be exacerbated by sleep deprivation, have been shown to negatively impact sperm count and quality. Chronic stress has been linked to lower testosterone levels, decreased sperm production, and decreased sperm motility.