Azoospermia is divided into two broad categories, obstructive azoospermia and non-obstructive azoospermia (OA and NOA). It is again important to note that this different from no sperm in the ejaculate secondary to a low or no volume ejaculate. Azoospermia can exist as a separate issue concurrently with a low volume ejaculate, and a low-volume ejaculate doesn’t necessarily mean that there is azoospermia. [link to low sperm count, low volume ejaculate subsection]
Non-obstructive azoospermia is more common than obstructive azoospermia. We will discuss both below.
Obstructive azoospermia (OA)
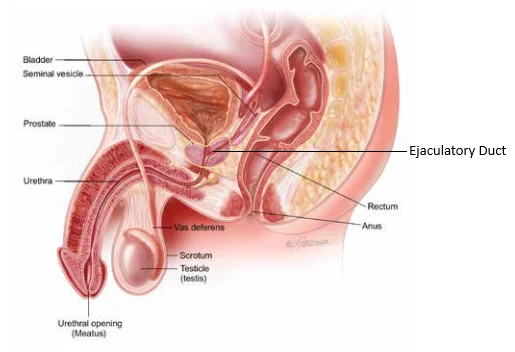
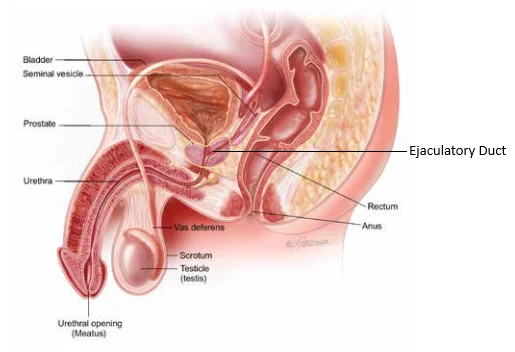
Obstructive azoospermia, or OA, is defined by the lack of sperm in the semen secondary to an obstruction of the vas deferens or full obstruction of the epididymis. This can either be congenital or acquired. The most common reason for congenital azoospermia is secondary to a defect in the cystic fibrosis gene, and this accounts for approximately 2 out of 3 cases. This doesn’t necessarily mean that a man has cystic fibrosis. A man can have only one altered copy of the cystic fibrosis gene, and as such he would have no evidence or clinical manifestations of the disease known cystic fibrosis. However, he may be missing part or all his vas deferens, the tube that carries sperm from the testes to the rest of the genitourinary tract (see above).
Acquired OA can also occur throughout a man’s life. The three most common reasons are vasectomy, hernia surgery, and infection. Vasectomies can sometimes be reversed, while other times though they may be able to be reversed it may not be the best choice for the couple.
Hernia repair is an underrecognized cause for OA. For hernia repair to cause azoospermia, the hernia operation would need to be done on both sides, or if a single functioning testicle on that side, and the complication of vasal obstruction would need to occur. As most hernia repairs are done past the reproductive age of most men, usually this is not discussed as a possible complication of the surgery.
While it is relatively common to get an infection in the genitourinary tract, it is rare but possible for certain types of infections to lead to OA. Giving a good, thorough history to your physician is important to recognizing this as a possible consequence.
Non-Obstructive Azoospermia
Non-obstructive azoospermia, or NOA, by contrast is not due to a blockage of the vas but rather secondary to a production defect in the testicle itself. It affects about 1% of the population. It is more common than obstructive azoospermia (OA). Though many patients can understand the process of OA better secondary to its straightforward nature, the processes for NOA are more complex and therefore there is a temptation for many patients and even some physicians to assume that azoospermia is by default OA. However, most azoospermia seen is not due to an obstruction but rather a defect in the production of sperm.
However, the good news is that most men with NOA can still produce very small quantities of sperm, and with the help of a trained Reproductive Urologist/Andrologist that sperm can be procured and used for assisted reproduction. It is important to note that to get this sperm is a complex process, often requiring the use of medications to stimulate production in the testes to optimize the chances of success, and specialized microsurgical techniques to get the most sperm possible while causing the least amount of damage within the testicle. The final part of this process, if successful in obtaining sperm, is to work with a facility that is familiar with using testicular sperm for the process of in vitro fertilization (IVF).
NOA can also be congenital or acquired. Congenital reasons for NOA are genetic in nature. Every year we find more genes that can be responsible for NOA either directly or indirectly. However, even with the impressive amount of knowledge we have acquired, we still only can identify the genetic reason behind 3-10% of all causes of NOA by commercially available testing.
Some known genetic causes are:
- Klinefelter’s syndrome: Most men have one X and one Y chromosome. Klinefelter’s syndrome is the presence of at least one more X chromosome than normal. This can lead to the predisposition to many diseases, as well as NOA
- Gene translocations and deletions: Sometimes a segment of a chromosome can “jump,” or translocate, to another chromosome during the fertilization process. This can lead to a normal set or slightly abnormal set of total genes, so development can be completely normal or only slightly abnormal, but during the development of sperm this causes dysfunction and inability for sperm to form
- Y-chromosome microdeletions: The Y chromosome is the smallest and encodes for many of the genes that give males their characteristics. In some men, a very small part of this gene can have missing parts. This may lead to NOA and depending on the region missing there may or may not be methods to salvage sperm for use with IVF.
Some of the above conditions can be tested with a Karyotype and a Y-chromosome microdeletion test. These tests are easily commercially available, and the price of testing has decreased dramatically over the past 10 years.
There are tests to verify other genetic conditions that can cause NOA. These tests are usually not performed on every patient with NOA as the costs can sometimes be prohibitive. Usually, a specialist such as a Urologist with specialization in male infertility will order these tests based on what findings they may encounter with labs, history, and physical exam. However, if there is evidence on this workup that the characteristics of certain disease processes exist, then these tests can be performed. Some examples include:
- Androgen Receptor testing (AR gene testing)
- Kallman’s Syndrome
- TEX11 gene testing
Some of these tests are ordered with what is known as Next-Generation Sequencing (NGS). NGS is not usually done for all men that have NOA but can be performed if there is evidence of a specific clue that warrants further study.
Depending on the results of a genetic test, these can then be used to make predictions on the chance of success with various specialized techniques.
Although all these tests are available, for most patients there is no current positive genetic test that can be identified as the reason for NOA. However, this does not mean that there is no genetic reason for infertility, but rather there is none that we can identify with commercial testing.
It is not recommended to use generic approaches to genetic testing for every man with NOA (e.g. 23andMe or Ancestry.com specialized testing services). This can lead to additional worry about a finding that may not be relevant, or increasing costs to the patient with additional testing that may not have any clinical relevance.
Acquired Non-Obstructive Azoospermia
For some men, NOA can be acquired as well. The most common cause of this is testosterone replacement. Testosterone replacement can act as a fairly effective male contraceptive, and the longer a patient is on testosterone, the harder it is to get sperm back. For a very small minority of men on testosterone long-term, this can even be irreversible.
Some other causes of acquired NOA include:
- Spinal Injury
- Neurologic disease
- Systemic chronic illness (e.g. liver failure, collagen vascular disease, autoimmune disease)
- Chemotherapy
This is by no means an exhaustive list, but rather highlights the importance of addressing fertility issues as soon as a medical condition arises and the man still desires to be fertile.
Techniques for sperm retrieval
Even though technically the definition of azoospermia means that there is no sperm in the ejaculate, often we are successful in obtaining sperm to be used for assisted reproduction. By using techniques listed below, depending on the type of azoospermia successful sperm extraction can be performed.
Sperm obtained from extraction can only be used in conjunction with In-Vitro Fertilization (IVF). More specifically, sperm obtained from these procedures can be used for what is known as Intracytoplasmic Sperm Injection (ICSI).
Microsurgical Testicular Extraction
Microscopic testicular sperm extraction (microTESE) is a surgical technique used to retrieve sperm from the testes of men who have non-obstructive azoospermia, which is a condition in which there are no sperm present in the semen.
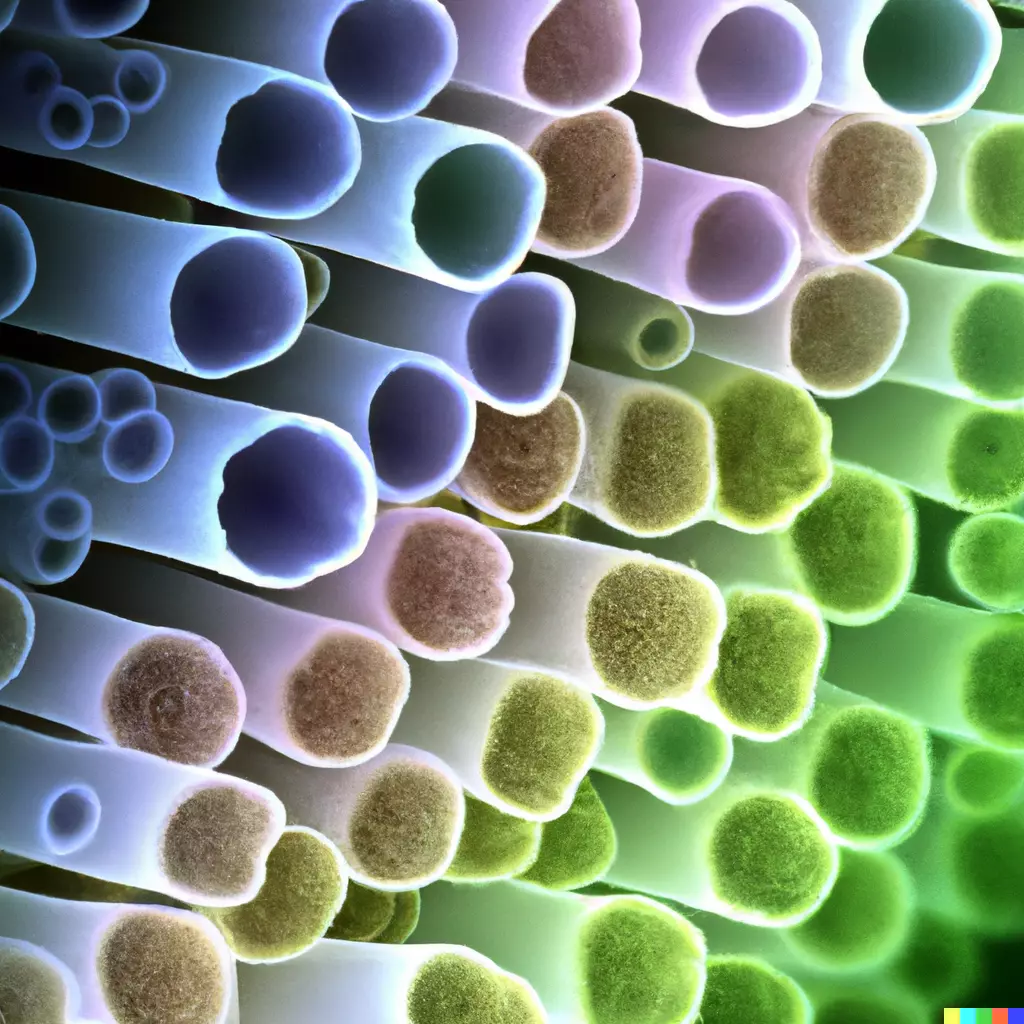
MicroTESE involves the use of a high-powered surgical microscope to identify and remove small tubules from within the testes that are more likely to contain mature sperm. The procedure involves making a small incision in the scrotum to access the testes.
Once the tubules have been removed, they are passed to an embryologist, who uses a microscope to identify and isolate individual sperm cells. The embryologist then prepares the sperm cells for use in assisted reproductive techniques such as in vitro fertilization (IVF) or intracytoplasmic sperm injection (ICSI).
MicroTESE is a highly specialized procedure that requires a great deal of skill and experience on the part of both the surgeon and the embryologist. The surgeon must have a thorough understanding of testicular anatomy and be able to identify the tubules that are most likely to contain mature sperm. The embryologist must also have extensive training in sperm retrieval and manipulation techniques.
One of the main challenges of microTESE is that the procedure can be time-consuming and technically demanding. The surgeon may need to spend several hours carefully searching for tubules that contain viable sperm. Similarly, the embryologist may need to spend several hours searching for and isolating individual sperm cells.
Despite these challenges, microTESE has been shown to be a highly effective technique for retrieving viable sperm from men with non-obstructive azoospermia. Studies have reported sperm retrieval rates of up to 60-70% with microTESE, which is significantly higher than other techniques such as conventional testicular sperm extraction (TESE).
Testicular Sperm Extraction
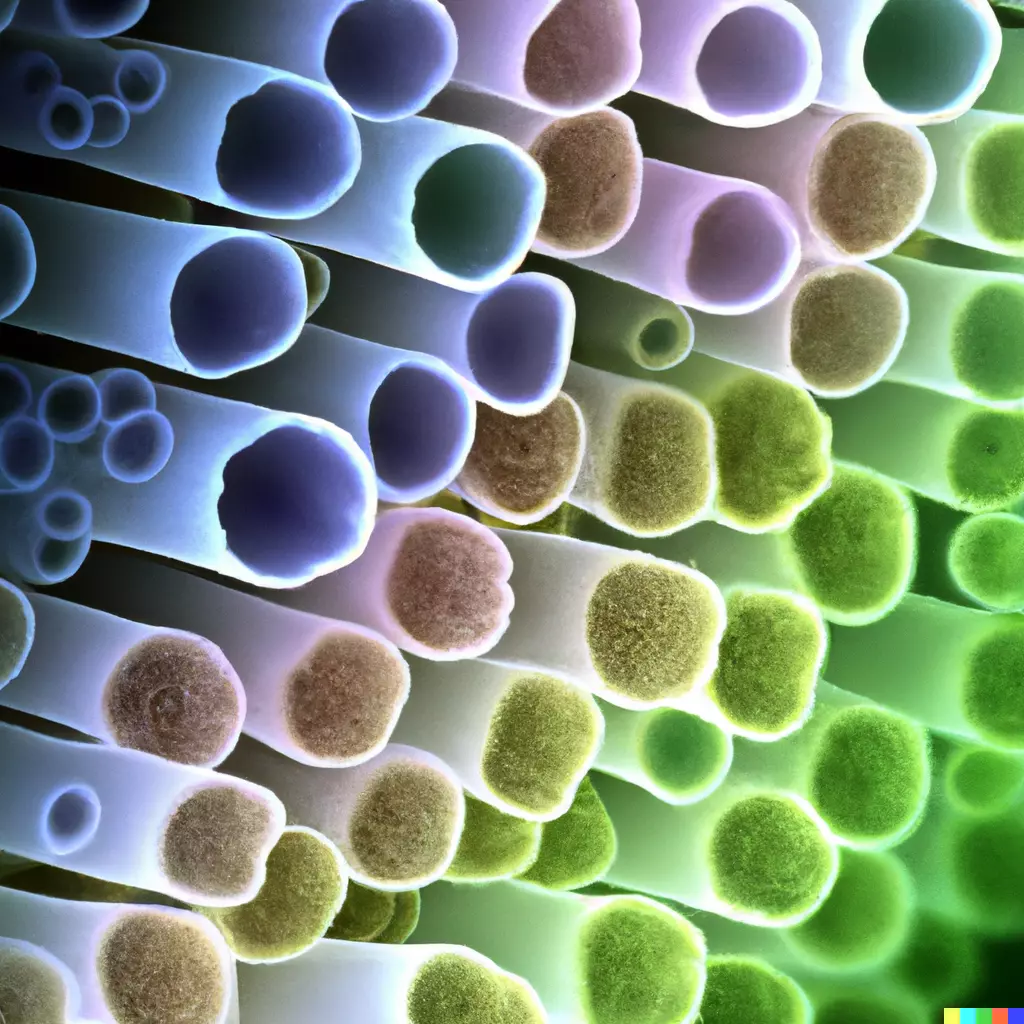
Testicular sperm extraction (TESE) is a surgical procedure that involves the removal of a small piece of testicular tissue to retrieve sperm for use in assisted reproductive techniques. TESE is typically used in cases of obstructive azoospermia, which is a condition in which there is a blockage in the male reproductive system that prevents sperm from reaching the semen.
During a TESE procedure, a small incision is made in the scrotum to access the testes. The surgeon then removes a small piece of testicular tissue, which is sent to an embryologist for examination. The embryologist then uses various techniques to isolate and retrieve viable sperm from the tissue.
TESE differs from microTESE in that it does not involve the use of a microscope to identify and remove specific tubules from within the testes. Instead, TESE involves the removal of a larger piece of testicular tissue, which may contain a mix of different types of tubules. While TESE can be effective in retrieving sperm from men with obstructive azoospermia, it may be less effective than microTESE in cases of non-obstructive azoospermia.
TESE can also be used in cases of cryptozoospermia, which is a condition in which there are very low levels of sperm present in the semen. In these cases, TESE may be used to retrieve viable sperm for use in assisted reproductive techniques such as IVF or ICSI.
TESA (Testicular Sperm Aspiration) is similar to TESE but involves the removal of sperm by aspirating with a needle. While both techniques can be effective in retrieving viable sperm, TESE is generally considered to be superior to TESA for several reasons.
TESE typically yields a higher number of viable sperm compared to TESA. This is because TESE involves the removal of a small piece of testicular tissue, which contains a higher concentration of sperm compared to the more limited amount of tissue that can be extracted during a TESA procedure.
Epididymal Sperm aspiration techniques
Epididymal sperm extraction (ESE) is a surgical technique used to retrieve sperm from the epididymis, a tube located behind each testicle that stores and transports sperm. ESE is typically used in cases of obstructive azoospermia, where there is a blockage in the male reproductive system preventing sperm from reaching the semen.
There are several different ESE techniques, including percutaneous epididymal sperm aspiration (PESA), and microsurgical epididymal sperm aspiration (MESA). PESA involves inserting a fine needle directly into the epididymis to aspirate sperm, while MESA involves a microsurgical approach to identify and retrieve sperm from the epididymis.
While ESE can be effective in retrieving viable sperm, it is generally considered to be inferior to testicular sperm extraction (TESE) for several reasons. First, ESE typically yields a lower number of viable sperm compared to TESE, which can make it more challenging to achieve a successful pregnancy. Additionally, the quality of epididymal sperm is generally considered to be lower than that of testicular sperm, with a higher proportion of abnormal or immature sperm that may be less suitable for use in IVF.