Female stress incontinence occurs most commonly with cough, laugh, or exercise/physical exertion. The reason this happens is because of a failure for the urinary sphincter to hold the urine in the bladder against the pressure that is being put on the bladder.
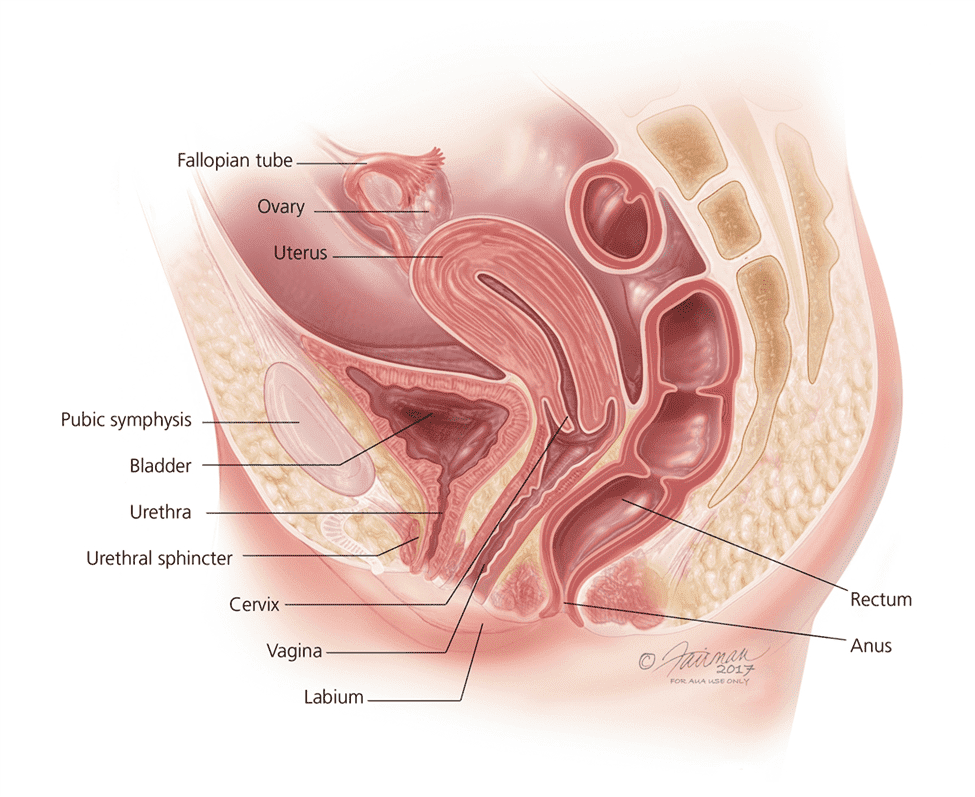
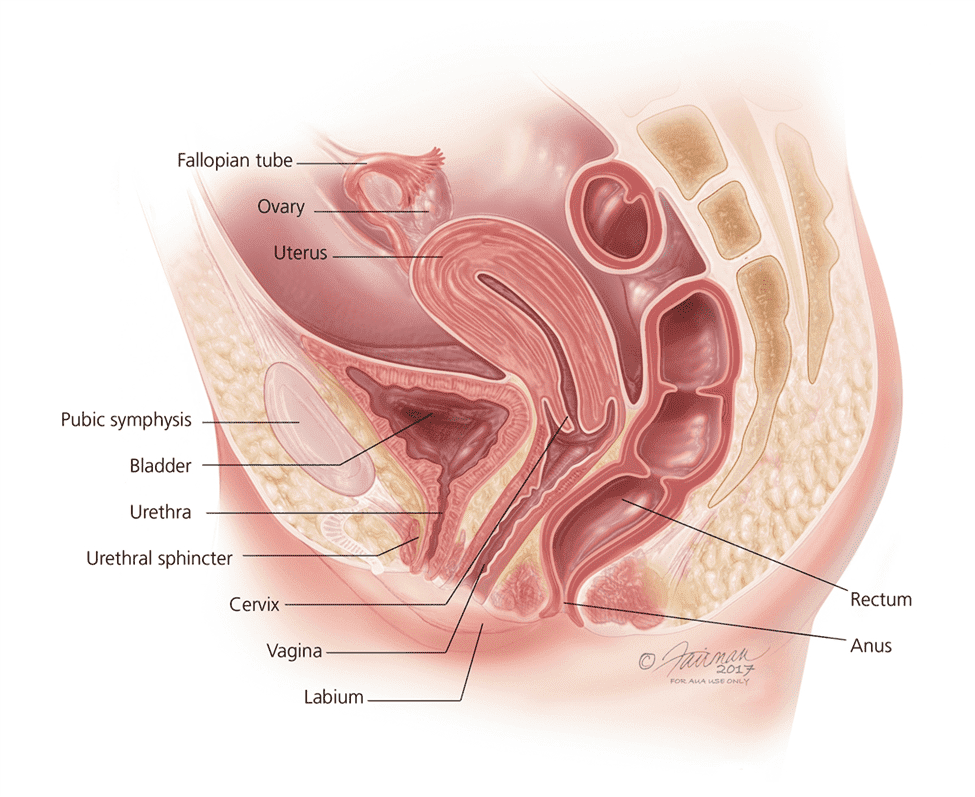
There are multiple reasons this happens. Think of the top of the female vagina as a hammock. That hammock has two points of attachment, the pelvic bone in the front and the uterus in the back. The threads of that hammock can get stretched with weight or childbirth, and those threads depend on estrogen to keep from falling. As women age, estrogen levels deplete, and during menopause that depletion can be somewhat rapid. This means those threads can loosen, allowing the top part of the vagina to fall. If a woman has had a hysterectomy, that is like one of the attachments of that hammock is faulty, allowing the whole hammock to fall forward. This can also lead to what is known as a cystocele, or a falling bladder into the vagina.
That hammock, or the roof of the vagina, also serves a role to provide a backboard to the urethra. The urethral sphincter, what is responsible for continence, is a circular muscle. When it contracts, it closes the urethra, and holds urine in place. However, it needs to have a strong backboard to close against, if the backboard has weakened then that sphincter does not have something helping it close well, and with enough pressure urine will leak.
Another potential issue is if the urethral sphincter itself gets damaged or loses potency, where the muscle isn’t as strong or cannot contract like it once did. This is known as intrinsic sphincter deficiency.
Your urologist may ask how many sanitary pads you use during the day to get a sense of how bad the stress incontinence is and may do diagnostic procedures such as cystoscopy and/or urodynamics to get a sense of anatomy and see what other reasons there may be for your incontinence.
To fix this issue, you can either strengthen the urethra and the muscles around it, provide a new, stronger backboard for the urethra to work, or make it easier for the urethra to close.
Pelvic floor exercises
A first option is to train and improve pelvic floor muscles to handle more stress. This is known as pelvic floor rehabilitation and can be like exercises done for urge incontinence, though work for a very different reason. Most women are familiar with similar exercises after childbirth, known as Kegel exercises. These types of exercises are done to restore the damage done to the pelvic floor after childbirth and can also be useful when these symptoms happen at another time in life. Your urologist may also refer you to a therapist that specializes in pelvic floor rehabilitation techniques. Other exercises are outlined below:
https://www.urologyhealth.org/healthy-living/care-blog/kegel-exercises-for-incontinence
Bulking Agents
Another useful intervention that can be done in combination with pelvic floor exercises is to lessen the amount of work that the sphincter needs to do by adding a bulking agent. Bulking agents are injected by cystoscopy, where a camera with an operating channel is used to pass a needle into the area around the bladder neck to add bulk and decrease the size of the hole that the urethra needs to close. Older bulking agents tend to be less effective than newer agents that maintain form for longer and do not dissipate as easily. Older agents need to be reapplied on average every 5 years, though newer agents are likely to last longer with better efficacy.
https://bulkamid.com/en-US
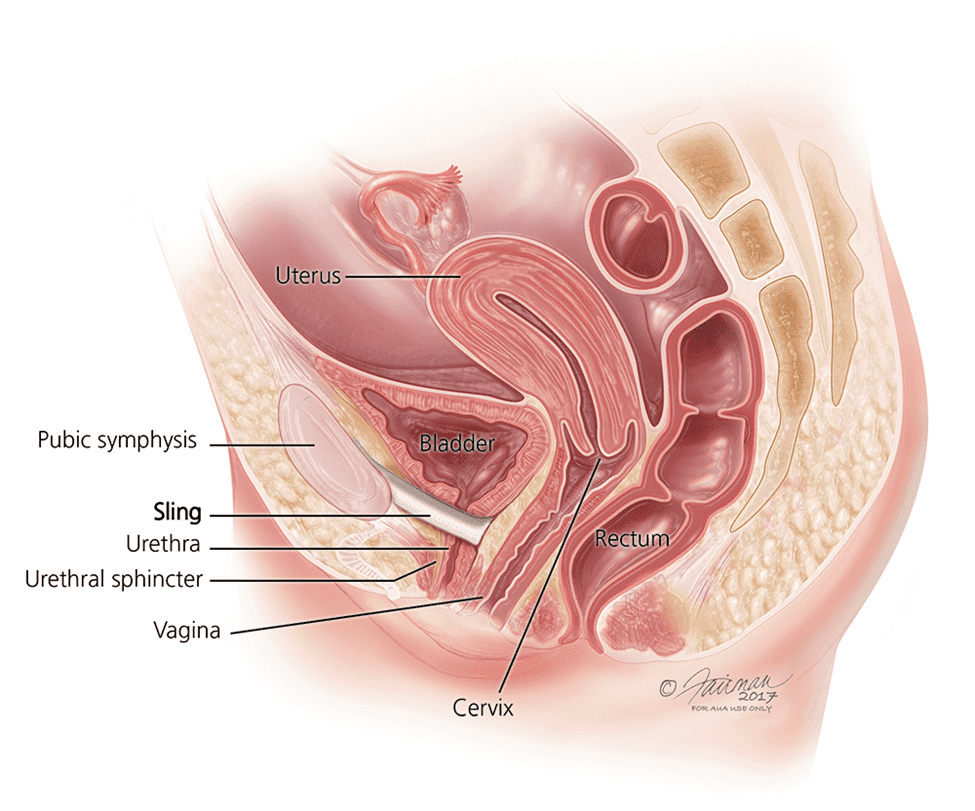
Urethral Sling
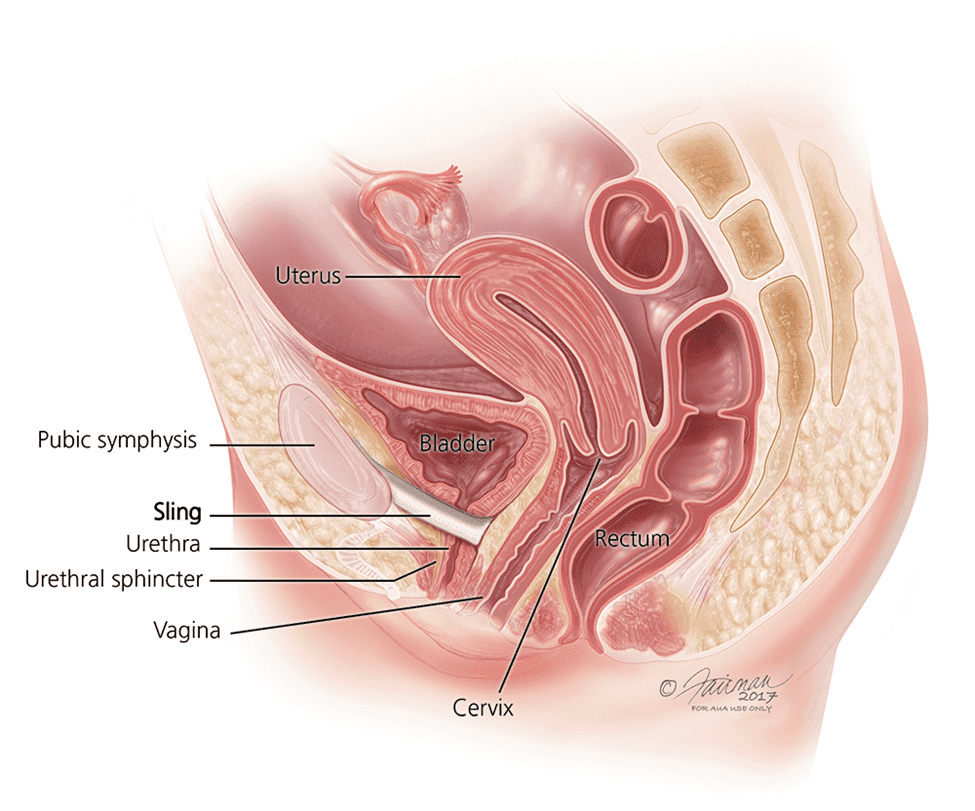
A urethral sling is a ribbon of material, either synthetic or biologic (made from a human or animal) that is placed below the urethra to give a backboard to the urethra. This can be a very effective way to stop potential leakage events.
The surgery is done as an outpatient. The surgeon makes a very small incision in the vagina, underneath the urethra, and creates tunnels on either side of the urethra to place the sling material. This can be done using the pelvic bone to either side of the urethra, known as a transobturator sling, or using the pubic bone on top of the urethra. With either approach, the point of the surgery is to provide a wall, or floor, that can adequately assist the sphincter to completely close the urethra and prevent leaking with cough, laugh, or exercise/movement.
The risks of surgery are a sling that is too tight and can cause urinary retention. Also, during the procedure, there can be damage to the urethra or bladder, and if this happens the surgeon may elect to abandon the procedure and place a catheter for a period to allow for the injury to heal. Also, there can be pain associated with the sling material, a rare complication that sometimes leads to the material having to be removed. Finally, sometimes the sling material can erode through the vaginal skin, especially if it is misplaced or the patient undergoes another surgery, which can lead to the surgeon taking out the sling material.
Traditional surgical approach
Though rarely performed with the current advances in slings and urethral bulking agents, occasionally there may be a need for the physician to perform a more traditional surgery to suspend the urethra effectively. There are many traditional approaches, including procedures that are vaginal as well as approaching from the abdomen. Most of these approaches use sutures to suspend or fix the urethra to allow for aid in closing. They are considered more invasive, and therefore with greater risk of side effects.
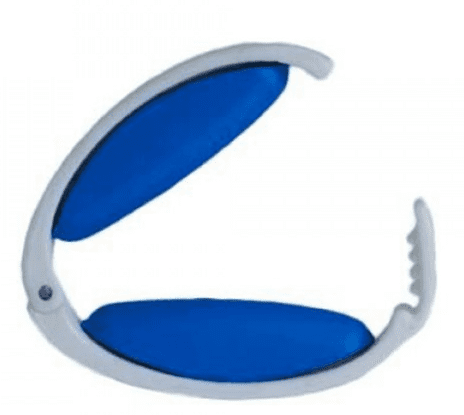
Artificial Urinary Sphincter (AUS)
An artificial urinary sphincter (AUS) is rarely used for female incontinence. This is usually reserved for the most complex reconstructions where there is little to no functional sphincteric muscle left, and usually this is in combination with a much larger procedure to reconstruct the bladder and pelvic floor. It consists of a circular balloon-type device that acts as a sphincter and is closed at rest. When the patient presses a pump in a separate location, this sphincter opens by fluid flowing out of the balloon (known as a cuff secondary to its physical appearance) to a reservoir, that automatically refills over the course of seconds (usually 45-60 seconds). This allows for the urine to flow out, and then continence is restored.
This will be detailed more in the discussion of male stress incontinence, as this is a much more likely scenario to need an artificial urinary sphincter (AUS).
Male Stress Incontinence
Males can also get stress incontinence, but for very different reasons. Male stress incontinence almost exclusively occurs when there is damage to the urethral sphincter responsible for urinary continence. This usually happens because of injury from a surgery, and usually from injury from prostate surgery or complications from radiation though it can happen from the need to open the urethra from scar as well. Very rarely, it can also be an early or late complication of incorrect catheter placement, which is why it is important for health care providers to follow strict rules for why and when to place a urinary catheter.
Whatever the reason, if the sphincter is unable to close the urethra completely, there can be leakage of urine. The goal of treatment is to allow for the urethra to close. There are non-surgical and surgical ways to do this. Surgically, this be done one of two commonly accepted ways, though there are more experimental approaches on the horizon.
Pelvic floor therapy
As with females, there is a role for pelvic floor therapy in males as well. This can be done with the help of a pelvic floor therapist. Exercises that can be done to improve pelvic floor strength can be found here:
https://www.urologyhealth.org/healthy-living/care-blog/kegel-exercises-for-incontinence
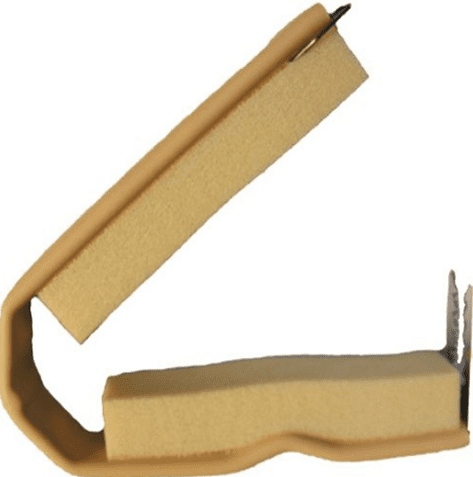
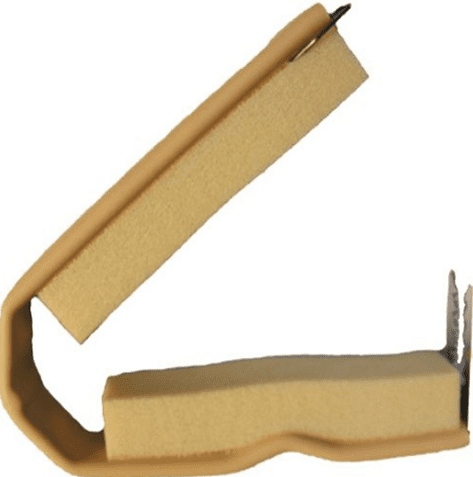
Incontinence Clamp
An Incontinence clamp is a device that essentially clamps the urethra externally by clamping the penis as a whole closed. The most commonly referred is a Cunningham Clamp, though there are others that work around the same basic principle. It is not meant to be worn 24/7. More appropriately, it is meant to be worn underneath underwear so that a man can go out of the house, exercise, travel, etc. without having to worry about leaking. When in a restroom the clamp is removed and the man urinates. Although the natural assumption is that a Cunningham clamp is uncomfortable, for most men that use the clamp it is usually comfortable enough to be worn daily without difficulty.
Cunningham clamps can be obtained without a prescription, and are usually inexpensive.
Male Urethral Sling
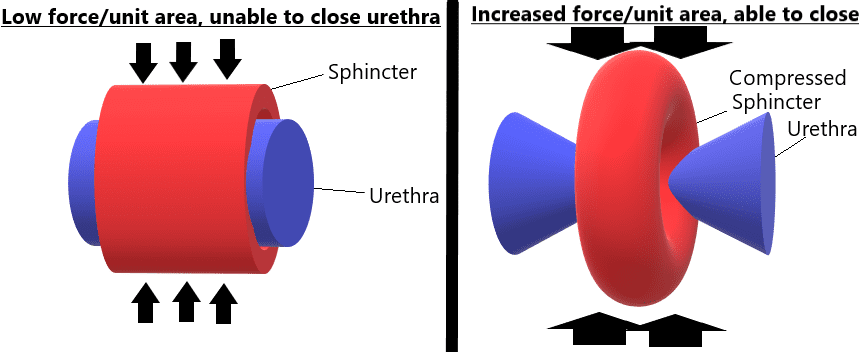
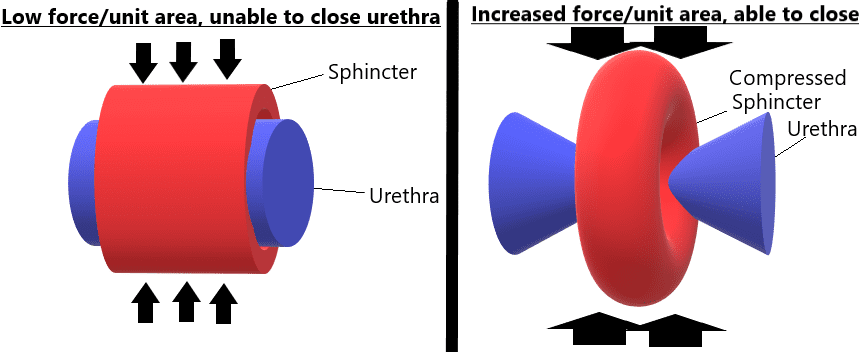
A male sling works on a very different concept than a sling for female incontinence. For females, the goal is to provide an effective backboard for the urethra to close adequately. For males, this is not the case. The sphincter is already compromised to some degree. The question is how much. If there is enough function left, the urethra can be compressed, and by compressing the urethra the sphincter may be more effective because the force per unit area can go up, as illustrated below:
Male sling placement is done as an ambulatory procedure. Patients typically go home that same day, and the biggest risk of the procedure is urinary retention, which happens in about 1 in 5 patients. This may require a catheter placed after the procedure temporarily, as most of these cases of retention resolve and do not require another surgery. Patient selection is very important, as there needs to be proof that the sphincter still has enough force to close the urethra, and the urethra is still pliable or soft enough to be closed. Sometimes, either after multiple surgeries or radiation treatment, the urethra may be too rigid to be closed by a native sphincter, especially if it is compromised.
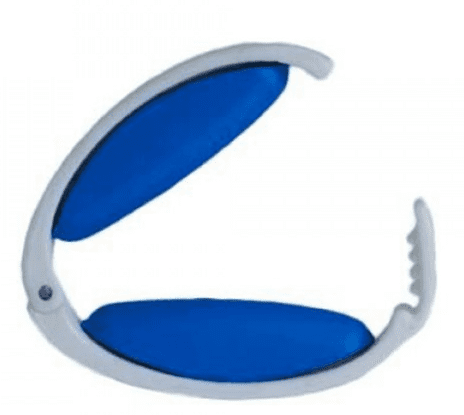
Artificial Urinary Sphincter (AUS)
As touched upon before, an AUS consists of a circular balloon-type device that acts as a sphincter and is closed at rest. When the patient presses a pump in a separate location, this sphincter opens by fluid flowing out of the balloon (known as a cuff secondary to its physical appearance) to a reservoir, that automatically refills over the course of seconds (usually 45-60 seconds). This allows for the urine to flow out, and then continence is restored.
_1696586342.png)
from healthline.com
An AUS can consist of a single cuff, or sometimes it is necessary to put two cuffs in series, known as a tandem cuff, to fully close the urethra. An AUS is considered the gold standard to treat male stress urinary incontinence.
Placement of an AUS sometimes is done with placement of a penile prosthesis, as often a male may have both urinary incontinence and erectile dysfunction after prostate surgery. For more information about penile prosthesis, please refer to information noted for erectile dysfunction located under the Men's Health section of the website.
The patient is obligated to be able to press the pump to use the AUS every time he urinates, however. This can sometimes be an issue as a patient ages, as patients with dementia or decreased ability to use their fingers are not candidates for an AUS.
Potential complications include damage to the urethra during surgery, in which case the procedure is usually aborted and a temporary catheter may be placed. However, long-term the biggest risks are infection and erosion. Because the AUS is a foreign object we implant in the body, if it becomes infected or exposed this usually requires prompt removal of the AUS components. Sometimes during the same procedure another can be placed, and sometimes there needs to be a period of recovery and/or antibiotics before reimplant can be considered.
This means that it is VERY important for a patient with an AUS to alert every health care provider that sees him that he has an AUS. It is not uncommon for a man with an AUS to arrive in the emergency room for an unrelated condition, and a catheter is placed by someone who does not know the patient has an AUS. This can lead to erosion and exposure of the cuff, as the cuff may not have been deflated before placement. This can lead to the need to replace the AUS with another surgery, and sometimes can lead to infections that can become life-threatening.



_1696586342.png)

